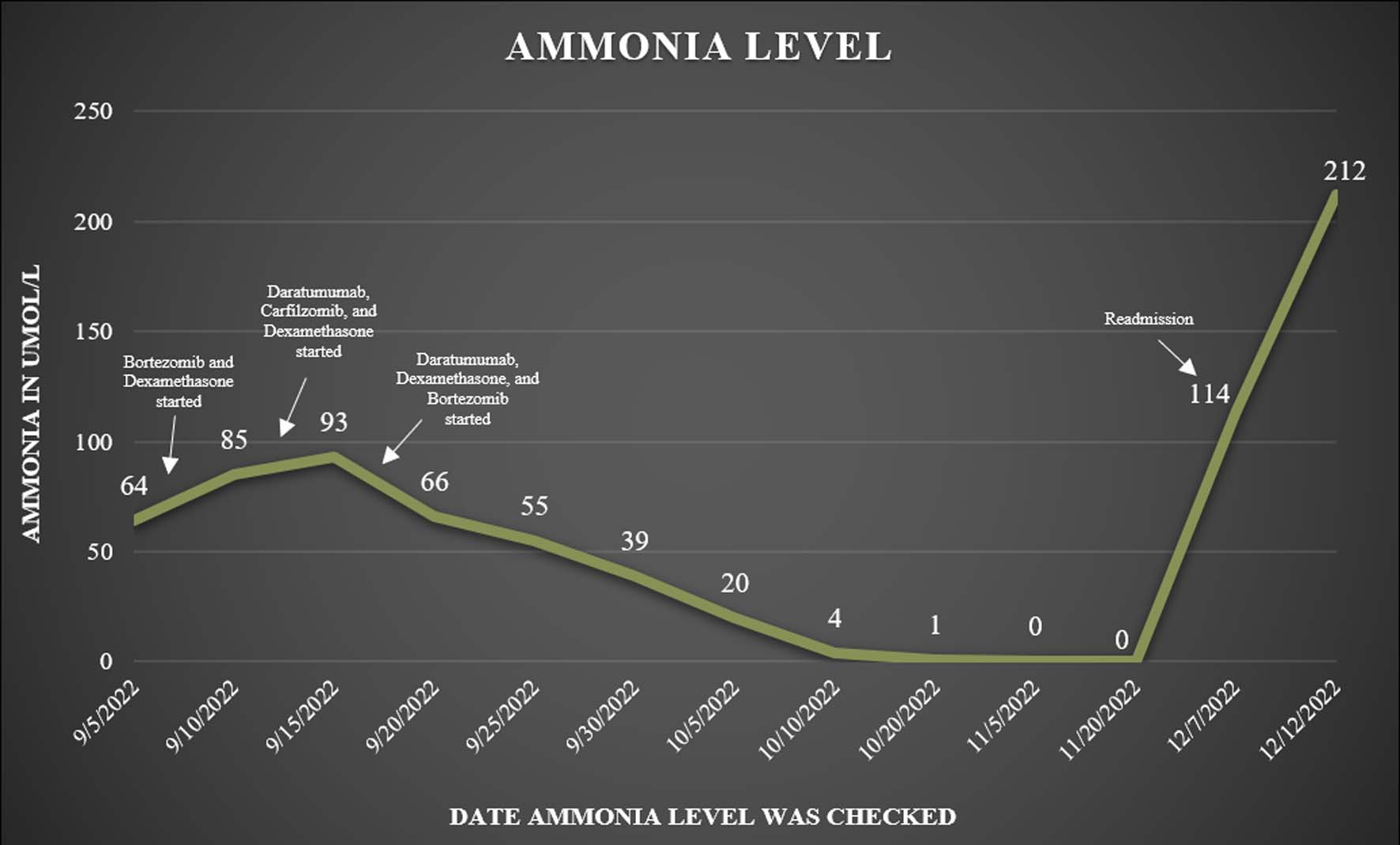
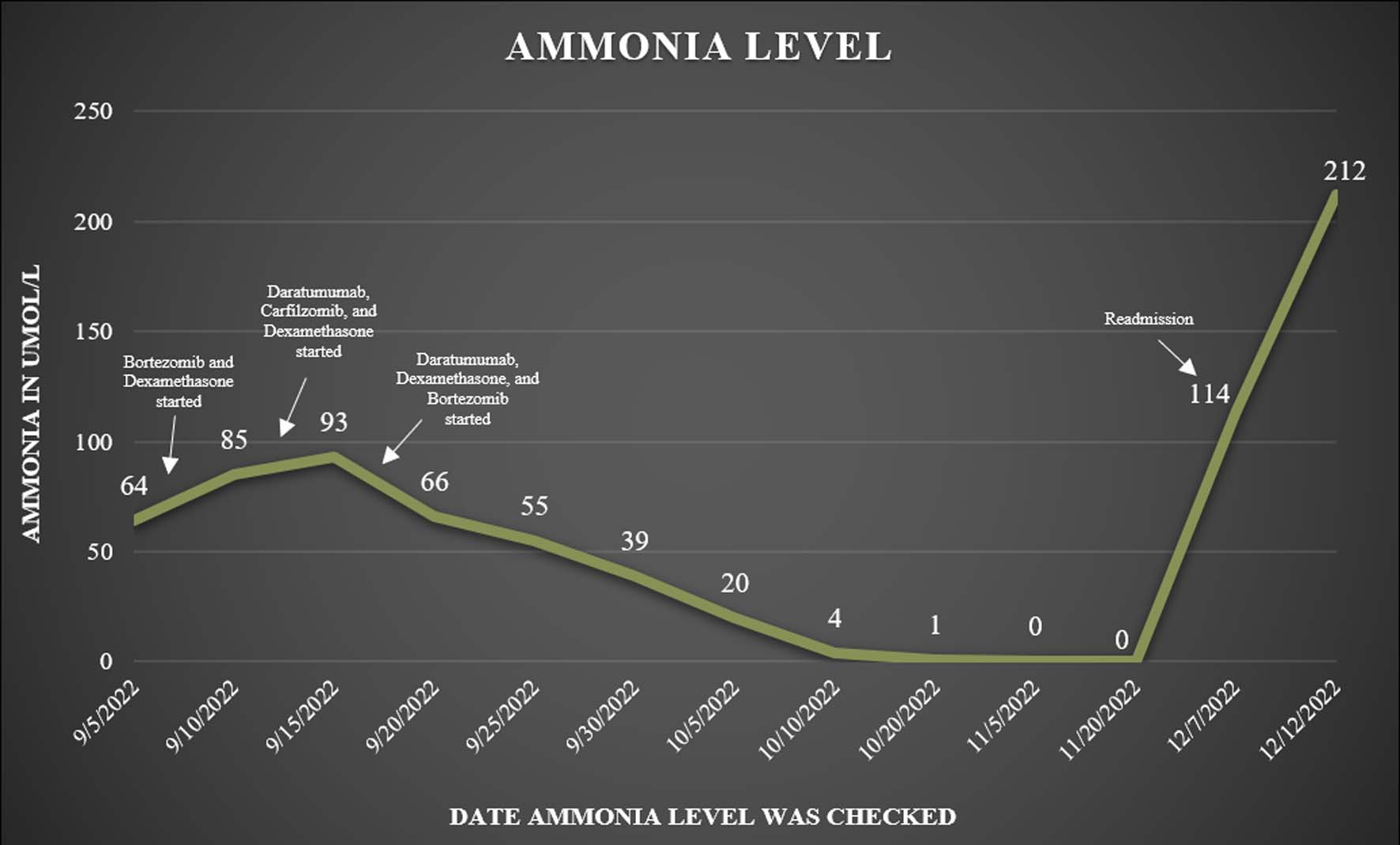
Figure 1. Patient’s ammonia levels recorded after discharge during his follow-up appointments.
| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 12, Number 3, June 2023, pages 128-132
Hyperammonemic Encephalopathy: A Rare Presentation of Relapsed Multiple Myeloma
Figure
Table
| Source | Initial treatment | Presenting symptom upon relapse | Ammonia levels | Outcome |
|---|---|---|---|---|
| MM: multiple myeloma; AMS: altered mental status. | ||||
| Douedi et al, 2021 [19] | A 51-year-old male was diagnosed with MM 6 years prior to relapse. He underwent four cycles of chemotherapy with ixazomib, darzalex, venetoclax and stem cell transplant 2 years prior to relapse. He was on maintenance therapy with daratumumab weekly with chronic dexamethasone. | After 6 years in remission, he presented to emergency department with radiating chest pain for 1 week and found to have a hemoglobin of 8 and platelets of 20, He was hospitalized and developed encephalopathy after 6 days. | The patient’s ammonia level was 118 µg/dL on development of encephalopathy, and eventually rose to 256 µg/dL. | He was intubated for airway protection due to encephalopathy, and ultimately chose to go to hospice after 2 weeks as he was unable to be weaned off the ventilator. |
| Murtaza et al, 2017 [12] | He was treated at time of diagnosis with hemodialysis to manage his renal failure and was treated with bortezomib and dexamethasone. He had relapse 1 year later and was treated with second-line chemotherapy with thalidomide and dexamethasone, but his disease continued to progress. He then started third-line therapy with lenalidomide and dexamethasone. Lenalidomide was held due to cytopenia. He continued to worsen over the next 2 years. He resumed on lenalidomide, but the disease progressed, so he was started on daratumumab, with dexamethasone, acetaminophen, and diphenhydramine. | He became lethargic after the first dose of daratumumab. Daratumumab was selected because of the patients cytopenia, and renal disease precluded alternatives. The patents rapidly declined and became unresponsive. | The patient’s ammonia level was 120 µg/dL initially; and rose to 127 µg/dL despite treatment. | He was treated with lactulose, rifaximin, vancomycin and cefepime and acyclovir but ammonia level slightly worsened and did not improve. The authors contemplated using cyclophosphamide but due to the patient’s poor prognosis with severe cytopenia and lack of response to treatment thus far made him a poor candidate. The family decided to withdraw care and the patient passed after 5 days of disease progression. |
| Nakamura et al, 2023 [20] | A 75-year-old female was initially treated with bortezomib-melphalan-prednisolone (VMP), lenalidomide-dexamethasone (Ld), pomalidomide-dexamethasone (Pd), bortezomib-dexamethasone (Bd), and panobinostat-bortezomib-dexamethasone, but had disease progression. | After disease progression on initial five therapies over 2 years and 3 months, the patient was started on carfilzomib-lenalidomide-dexamethasone (KRd). She developed encephalopathy 1 day later. | The patient’s ammonia level was 286.6 µg/dL. | The patient was treated with branched-chain amino acid (BCAA) agent for hyperammonemia and was continued on KRd treatment. Despite improvement in ammonia level, her MM progressed, and the patient ultimately died 7 days later. |
| Nakamura et al, 2023 [20] | A 61-year-old female had relapsed after 3 years following an MM diagnosis at age 55. The patient was initially treated with autologous peripheral blood stem cell transplant. She was then managed consecutively with Ld, Pd, daratumumab-bortezomib-dexamethasone, carfilzomib-dexamethasone, and ultimately elotuzumab-pomalidomide-dexamethasone (EPd) but still had disease progression. | The patient presented with altered mental status 5 days after EPd treatment. | The patient’s ammonia levels were 212.1 µg/dL on presentation with AMS. The patient was treated with BCAA agents, and ammonia level decreased to 56.7 µg/dL after 11 days. | The patient continued two additional cycles of EPd after development of hyperammonemia but ultimately deteriorated due to infectious complications, due to which she could not continue chemotherapy. She died 4 months after the finding of hyperammonemia. |
| Nakamura et al, 2023 [20] | A 48-year-old woman was initially treated with Bd, Ld, and Pd but continued to have disease progression. She then started on elotuzumab-lenalidomide-dexamethasone (ERd). | One day prior to starting on ERd, the patient developed altered mentation. She was started on ERd as planned and concomitantly treated for hyperammonemia with BCAA agents. | The patient’s ammonia level was 67.7 µg/dL | The patient had improvement in ammonia levels and corresponding improvement in encephalopathy after 2 days of treatment with BCAA agents. After one cycle of ERd she developed massive ascites and was found to have multiple metastases to the liver. She died from complications of refractory ascites 32 days following diagnosis of hyperammonemic encephalopathy. |