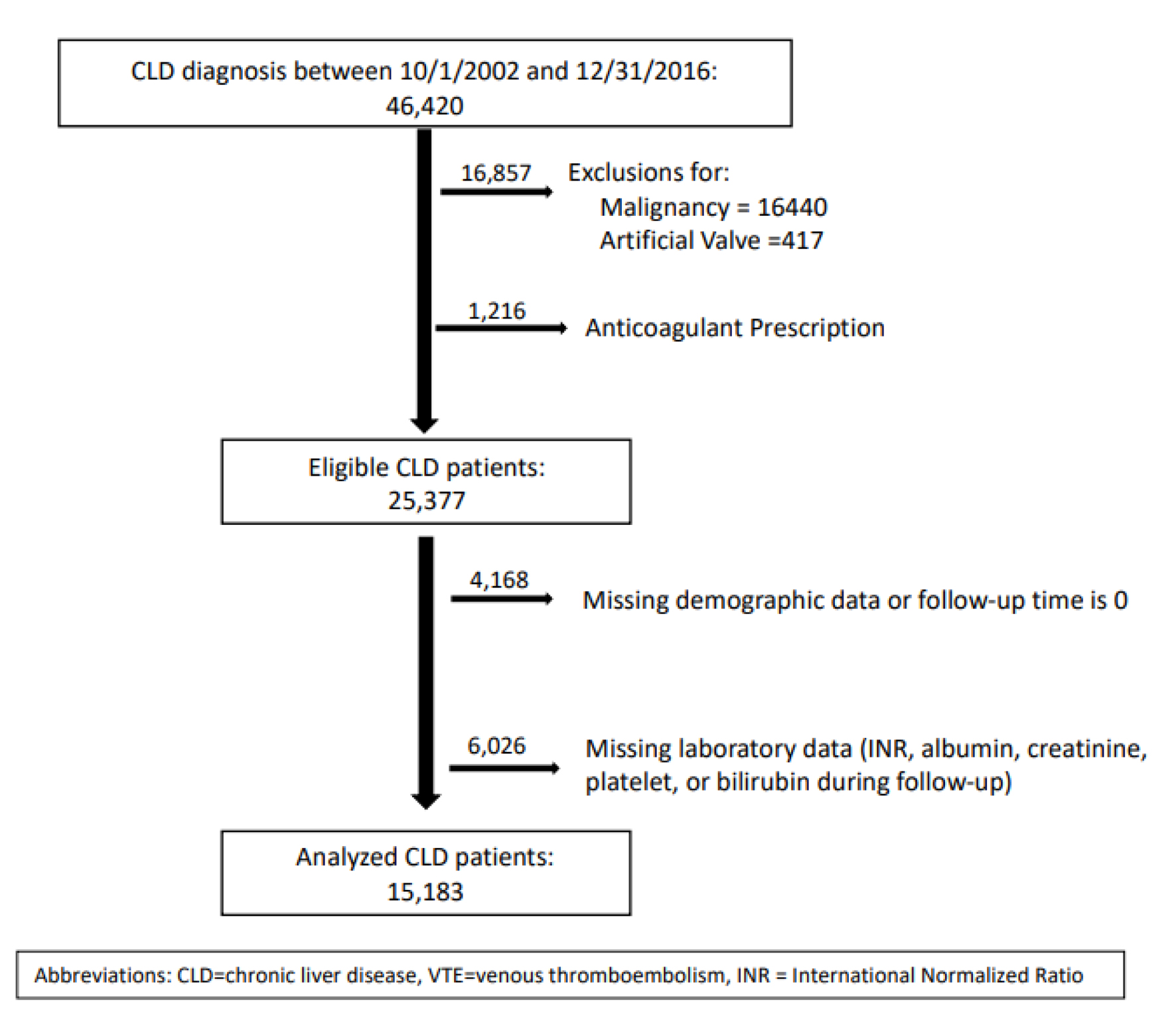
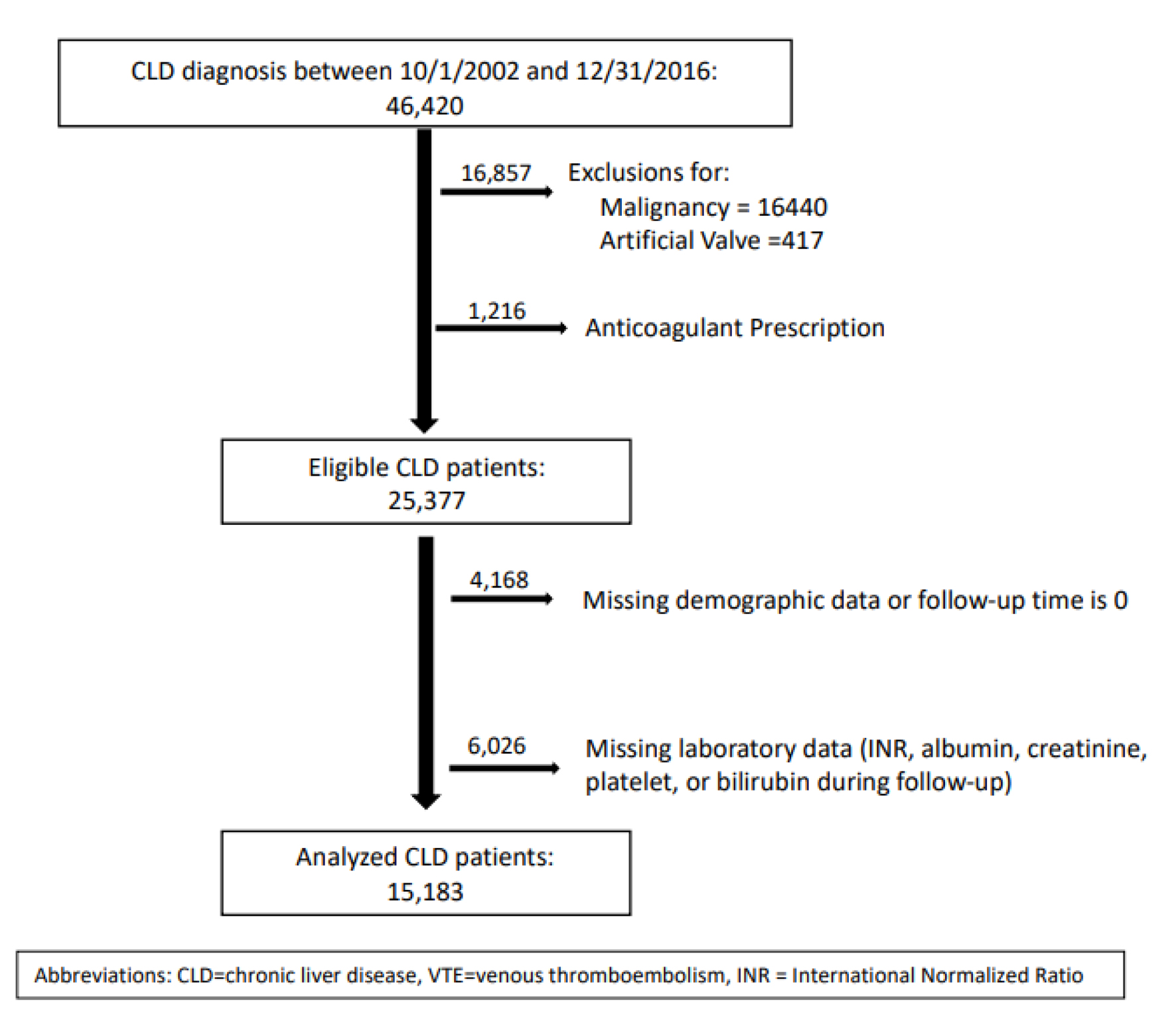
Figure 1. CONSORT diagram. CLD: chronic liver disease; VTE: venous thromboembolic; INR: international normalized ratio.
| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Original Article
Volume 13, Number 3, June 2024, pages 71-78
Predictors of Non-Variceal Hemorrhage in a National Cohort of Patients With Chronic Liver Disease
Figure
Tables
| Demographic/clinical characteristics | Total (N = 15,183) | P-value | |
|---|---|---|---|
| Hemorrhage (n = 674) | No hemorrhage (n = 14,509) | ||
| aChi-square test. bt-test. cWilcoxon two-sample test. | |||
| Mean age (years) | 57.3 | 58.2 | 0.02b |
| Male (%) | 97.3 | 97 | 0.58a |
| Race (%) | 0.02a | ||
| White | 82.1 | 85.6 | |
| Black | 14.1 | 11.9 | |
| Other | 3.9 | 2.5 | |
| Prior bleeding (%) | 8.9 | 8.2 | 0.48a |
| Cardiovascular disease (%) | 8.3 | 7.9 | 0.75a |
| Congestive heart failure (%) | 7.3 | 5.3 | 0.03a |
| Dementia (%) | 1 | 0.5 | 0.08a |
| Chronic lung disease (%) | 11.6 | 12.4 | 0.54a |
| Connective tissue disease (%) | 1.3 | 0.8 | 0.11a |
| Peptic ulcer (%) | 1.5 | 1.6 | 0.77a |
| Diabetes mellitus (%) | 22.3 | 24.4 | 0.21a |
| Hemi- or paraplegia (%) | 0.5 | 0.4 | 0.81a |
| HIV/AIDS (%) | 0.6 | 1 | 0.32a |
| Anemia (%) | 26 | 19.2 | < 0.001a |
| Alcohol abuse (%) | 38 | 30 | 0.001a |
| Ascites (%) | 5.3 | 4.2 | 0.15a |
| NSAID use (%) | 23.4 | 22.4 | 0.53a |
| Antiplatelet use (%) | 17.4 | 14.7 | 0.053a |
| Median platelet count (/µL) | 119,000 | 121,000 | 0.49c |
| INR (median) | 1.4 | 1.3 | < 0.001c |
| Median albumin (g/dL) | 2.8 | 3.1 | < 0.001c |
| Median bilirubin (mg/dL) | 1.9 | 1.6 | < 0.001c |
| Median creatinine clearance (mL/min) | 93.4 | 89.1 | < 0.001c |
| Infection (%) | 45.1 | 25.2 | < 0.001a |
| MELD score > 20 (%) | 14 | 12.8 | 0.0004a |
| Frequency/N (%) | |
|---|---|
| Total (any location) | 674 (4.4/year) |
| Upper gastrointestinal | 404 (60.0) |
| Lower gastrointestinal | 130 (19.3) |
| Intracranial | 67 (9.9) |
| Nasal/respiratory | 39 (5.8) |
| Genitourinary | 26 (3.9) |
| Peritoneum | 3 (0.4) |
| Hemorrhage, unspecified | 2 (0.3) |
| Joint/soft tissue | 3 (0.4) |
| Parameter | Adjusted hazard ratio | 95% confidence interval | P-value |
|---|---|---|---|
| aStudied as time-varying variables. bCollinearity was tested between these variables (tolerance > 0.92 and condition index < 5). AIDS: acquired immune deficiency syndrome; CrCl: creatinine clearance; HIV: human immunodeficiency virus; HTN: hypertension; INR: international normalized ratio; NSAID: non-steroidal anti-inflammatory drug; PPI: proton pump inhibitor; SBP: systolic blood pressure. | |||
| Age | 0.99 | 0.985 - 1.003 | 0.20 |
| Gender (Ref: male) | 1.36 | 0.84 - 2.20 | 0.22 |
| Race (Ref: Caucasian) | |||
| African American | 1.04 | 0.83 - 1.30 | 0.74 |
| Others | 1.54 | 1.03 - 2.28 | 0.03 |
| HTN (SBP > 160 mm Hg) | 1.36 | 0.98 - 1.89 | 0.06 |
| Albumin (≤ 3.5 g/dL)a, b | 3.68 | 2.84 - 4.77 | < 0.0001 |
| Anemiaa | 1.30 | 1.08 - 1.57 | 0.01 |
| Bilirubin (≥ 2 mg/dL)a, b | 1.45 | 1.19 - 1.76 | 0.0002 |
| Chronic kidney disease (CrCl < 30 mL/min)a, b | 2.63 | 2.05 - 3.39 | < 0.0001 |
| INR > 1.5a, b | 1.68 | 1.39 - 2.04 | < 0.0001 |
| Thrombocytopenia (platelets < 50,000/µL)a | 0.96 | 0.67 - 1.34 | 0.80 |
| Antiplatelet usea | 1.36 | 1.02 - 1.82 | 0.03 |
| NSAID usea | 1.21 | 0.75 - 1.96 | 0.43 |
| PPI usea | 1.23 | 1.05 - 1.43 | 0.01 |
| Prior hemorrhage (within 5 years) | 0.92 | 0.70 - 1.22 | 0.56 |
| Alcohol abuse | 1.29 | 1.10 - 1.53 | 0.002 |
| Ascitesb | 1.01 | 0.71 - 1.43 | 0.95 |
| Cardiovascular disease | 0.85 | 0.62 - 1.17 | 0.33 |
| Congestive cardiac failure | 1.17 | 0.84 - 1.62 | 0.35 |
| Chronic lung disease | 0.85 | 0.66 - 1.10 | 0.23 |
| Connective tissue disease | 1.51 | 0.74 - 3.08 | 0.25 |
| Dementia | 2.56 | 1.19 - 5.51 | 0.02 |
| Diabetes mellitus | 0.93 | 0.76 - 1.14 | 0.51 |
| HIV/AIDS | 0.57 | 0.22 - 1.51 | 0.26 |
| Hemi- or paraplegia | 0.89 | 0.27 - 2.89 | 0.84 |
| Peptic ulcer disease | 0.82 | 0.43 - 1.56 | 0.55 |
| Infections | 2.54 | 2.12 - 3.05 | < 0.0001 |