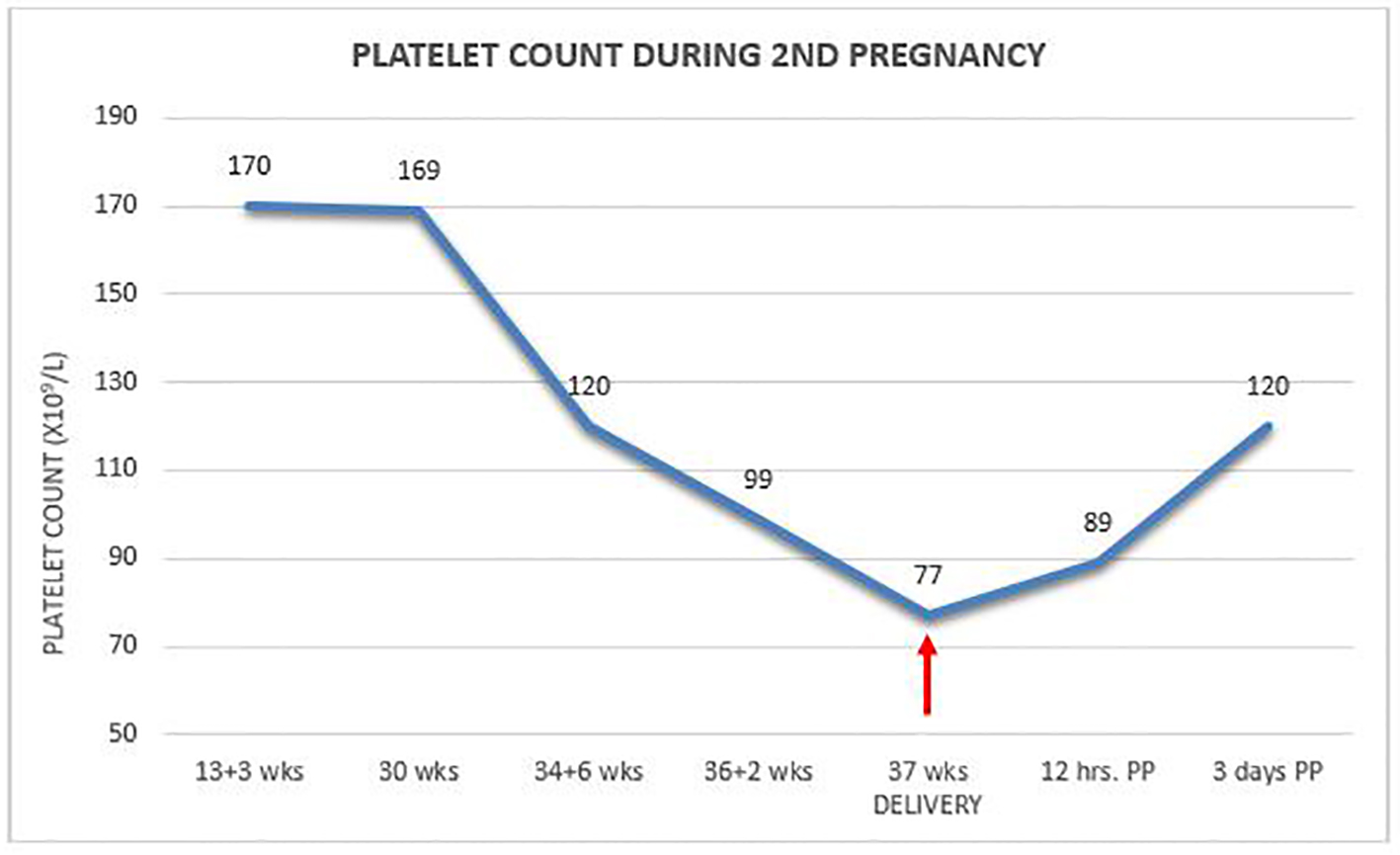
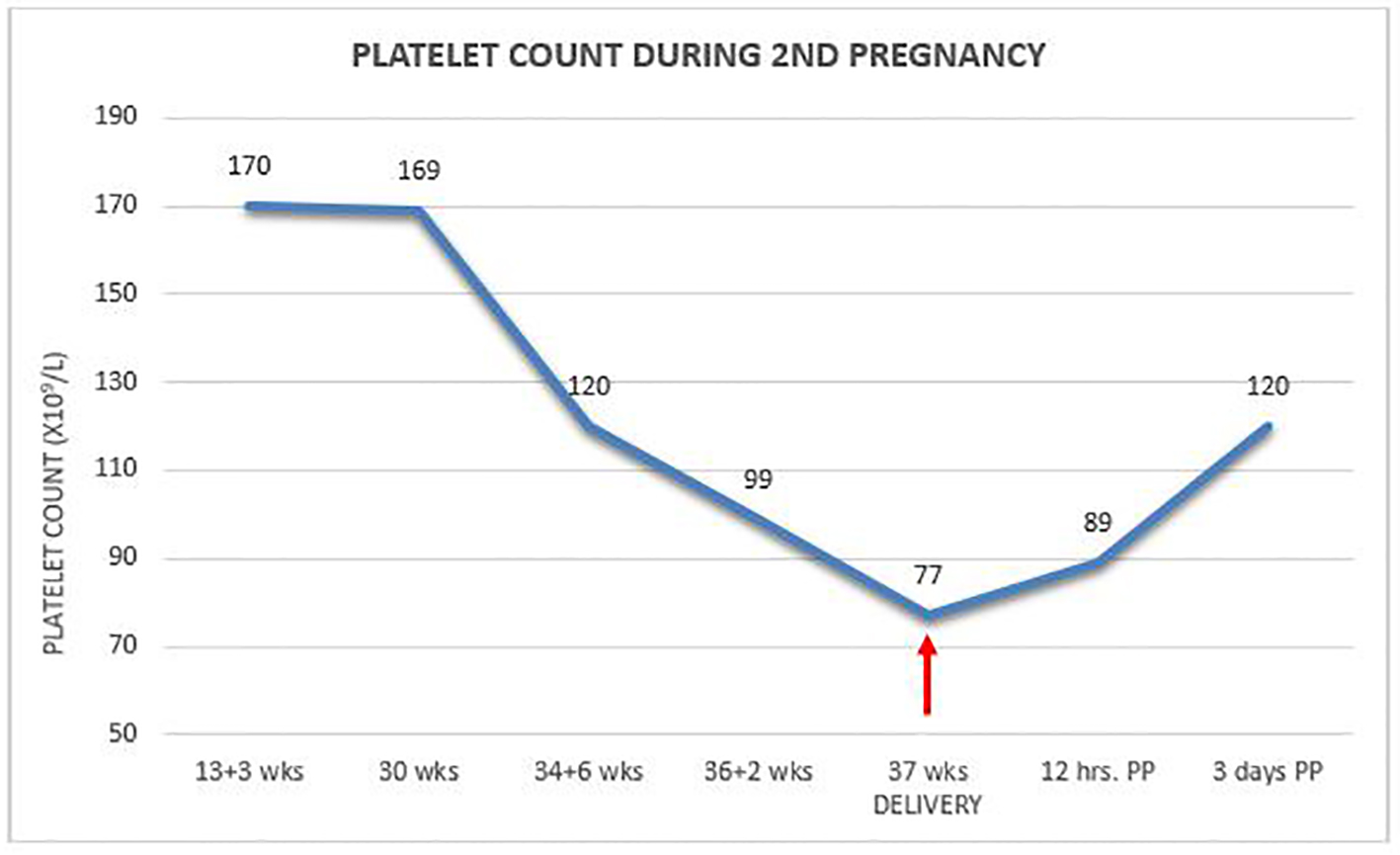
Figure 1. Platelet count during second pregnancy.
| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 5, Number 4, December 2016, pages 142-150
Severe Gestational Thrombocytopenia: A Case Report and Brief Review of the Literature
Figure
Table
| Features | Gestational thrombocytopenia (GT) | Immune thrombocytopenia (ITP) |
|---|---|---|
| *Diagnosis must be questioned if item was not fulfilled. | ||
| Peripheral blood smear examination (PBS) | Isolated TCP, abundant normal megakaryocytes, normal platelets of all generations while other cell-lines are normal* | Isolated TCP, abundant normal megakaryocytes, normal platelets of all generations while other cell-lines are normal* |
| Diagnosis | Exclusion of other causes of TCP [3] | Exclusion of other causes of TCP especially secondary ITP [3] |
| Past history | Negative before pregnancy* (except in previous pregnancy) | Mostly positive, but 30% of ITP cases might present for the first time during pregnancy (new-onset). |
| Timing of diagnosis | Might appear at any trimester but mostly during late second or third trimesters [11] | Can appear at any trimester but typically in early pregnancy [11]. |
| Platelet count trends | Decrease towards full-term if appeared early [24] | Decrease towards full-term in at least 50% of cases [16, 22]. |
| Multifetal pregnancy | Common association [11] | No reports of such predilection. |
| Postpartum recovery | Usually rapid and necessarily back to normal levels* | Recovery is usually slower and unlikely to normal levels* |
| Platelet count levels | Usually > 70 × 109/L but can reach lower levels [9] | Variable and can reach very low levels. |
| Predisposes to obstetric complications | None [10] | None [23]. |
| Maternal bleeding episodes | None reported even with low platelet counts* | Probable. New-onset cases of ITP might have higher rates of bleeding [6]. |
| Neonatal thrombocytopenia | Probable, reported rates (0.1-2%) similar to infants born to non-thrombocytopenic mothers [6, 8] though others reported higher rates [25, 27]. | Affects (25%) of cases but cannot be predicted and not related to maternal platelet count or antibodies titers [13]. |
| Neonatal bleeding | None [3] even in newborns with low platelet counts. | Can occur but uncommon [16] with serious bleeding as ICT only 1-2% [26]. |
| Response to steroids or IVIG treatment | No treatment is required. In the very few severe cases who received treatment, no response was elicited [18, 19]. | Response as in non-pregnant cases. Thirty to fifty percent of patients might require treatment [16]. More new-onset cases might require therapy [16]. |
| Recurrence in future pregnancies | Probable, but rate is unknown. | Probable, but rate is unknown. |