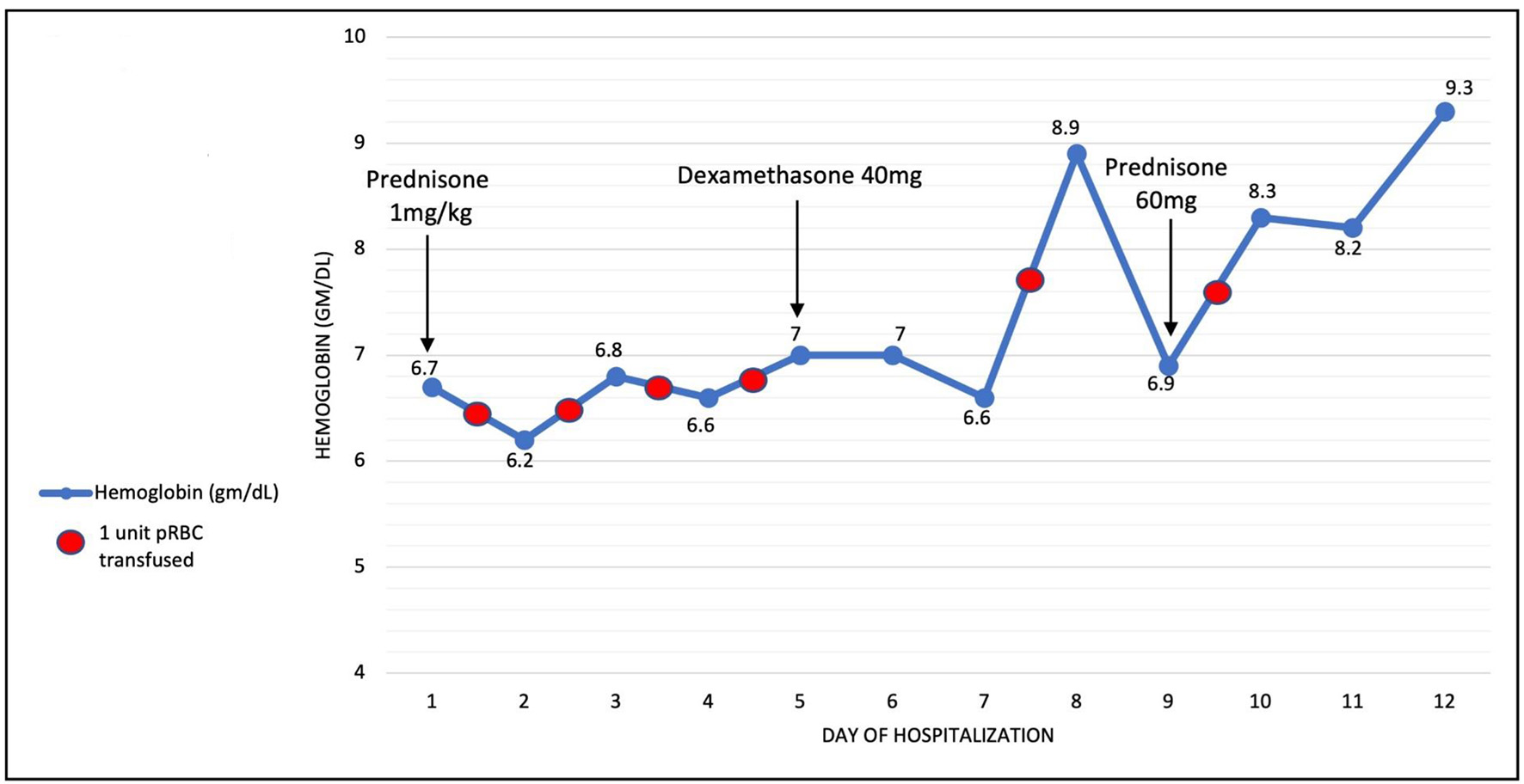
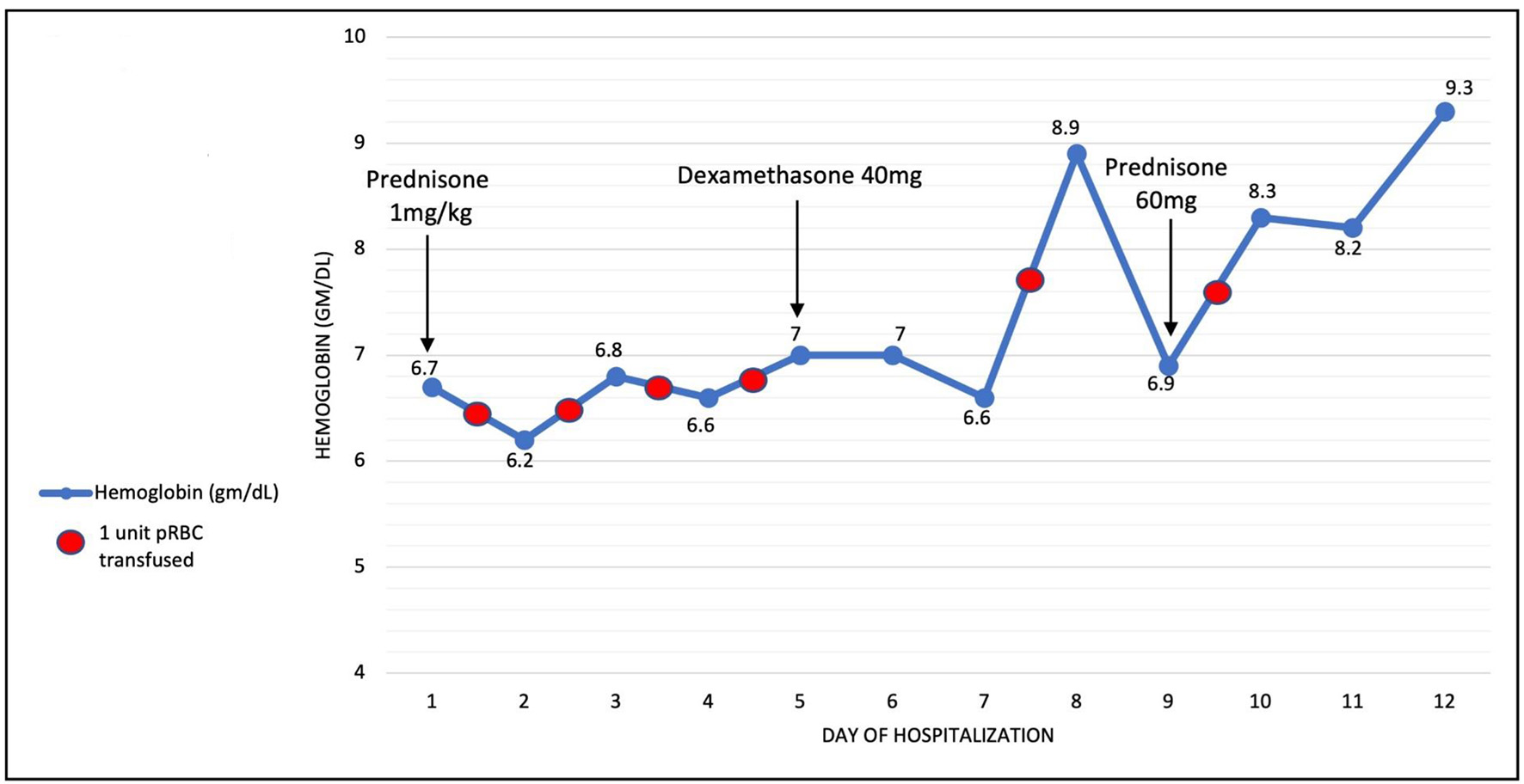
Figure 1. Hemoglobin throughout hospitalization. Arrows indicate start date of medications. Red circles indicate blood transfusion.
| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 10, Number 5, October 2021, pages 221-227
Hemolytic Anemia Complicating COVID-19 Infection
Figure
Tables
| References | No. of patients | Age | Median Hgb at diagnosis (g/dL) | AIHA type | Day of onseta | Underlying disease likely contributing | Treatment type | Time to remission and/or stabilization of Hgb |
|---|---|---|---|---|---|---|---|---|
| aDay of onset of AIHA from day of COVID diagnosis. +D1 defined as occurring on the day of COVID diagnosis. bOropharyngeal squamous cell CA on chemo-radiation; positive mycoplasma IgM: NEG PCR. cExact date of diagnosis not specified; Hgb ranged from 10.7 to 7.9 during hospitalization. dDate of COVID test not specified; coryzal symptoms started 2 weeks prior to COVID diagnosis. eCOVID diagnosis with thrombocytopenia was D+7 after respiratory symptoms started. AIHA occurred D+10 after COVID diagnosis (D+17 from onset of symptoms). fAsymptomatic COVID infection diagnosed same day as AIHA. gHgb = 8.1 on D6; Hgb = 12.6 at 7 weeks. hPatient discharged on day 8; Hgb was 11g/dL 7 days after discharge. iPrior history of AIHA, 3 years before COVID maintained on daily prednisone 20 mg. AIHA: autoimmune hemolytic anemia; IVIG: intravenous immunoglobulins; Hgb: hemoglobin; Hx: history; CLL: chronic lymphocytic leukemia; MZL: marginal zone lymphoma; MGUS: monoclonal gammopathy of unknown significance; TCP: thrombocytopenia; ITP: immune thrombocytopenic purpura; NA: not available. | ||||||||
| Campos-Cabrera et al [4] | 2 F | 35 and 58 | NA | Warm IgG + C3d | D+1 | None | Prednisone | NA |
| Capes et al [5] | 1 M | 62 | 6.9 | Positive C3b | D+16 | Questionableb | Transfusion support only (8 units over 1 week) | NA |
| Chiare et al [6] | 1 F | 86 | 8.3 | Positive IgG | D+49 | None | Steroids | D+13 |
| Hindilerden et al [7] | 1 M | 56 | 4.3 | Positive IgG + C3d | D+4 | None | IVIG then steroids | D+12 transfusion independent; D+14 Hgb 8.4; D+17 Hgb > 10.7 |
| Hseih et al (2021) [8] | 1 M | 84 | 4.4 | Positive IgG + anti-Kell | D+10-13 | None | Transfusion + steroids | NA |
| Huda et al (2021) [9] | 1 M | 54 | 9 | Positive IgG | D+8 | None | Prednisone | NA |
| Jacobs and Eichbaum [10] | 1 F | 33 | 1.3 | Positive IgG + C3; possibly mixed AIHA | D-2 | None | Steroids + rituximab + tocilizumab | D+10 |
| Jawed et al [11] | 1 M | About 50 | 7.9 to 10.7c | Positive C3d (did not specify if cold or warm) | NAd | None | NA | D+21 |
| Lazarian et al [12] | 7 (3 F, 4 M) + 1 with Hx of AIHA | > 60 | 7 | 4 with warm (2 IgG only, 2 IgG + C3d); 3 with cold (2 C3d only, 1 C3 + IgG) | Median + D9 (range 4 - 13) | 5 (CLL, MZL, MGUS) | Five treated with steroids; two treated with rituximab | NA |
| Li et al (2020) [13] | 1 M | 39 | 6 | DAT 3+ (did not specify if IgG or complement) | D+10e | None | IVIG only: patient had gastrointestinal bleed due to ITP treated with IVIG | D+28 (Hgb 7 after IVIG, Hgb 11 four weeks post discharge) |
| Liput et al [14] | 1 F | 33 | 6.5, nadir 6.2-transfused | Positive IgG + C3 | D+1f | None | Prednisone | Not reportedg |
| Lopez et al [15] | 1 F | 46 | 9.7 | Warm (positive IgG + C3) | D-3 | Congenital TCP | Prednisone after IVIG | D+15h |
| Patil et al [16] | 1 F | 51 | 5.1 | Positive C3d; cold agglutinin titer 80 | D+1 | None | Solumedrol for respiratory deterioration | D+14 (Hgb 11) |
| Raghuwanshi [17] | 1 M | 45 | 6.9 | Cold agglutinin | D+1 | None | NA | NA |
| Ramos-Ruperto et al (2021) [18] | 3 (1 M, 2 F) | 54, 72,76 | 6.5 - 8 | 2 with positive IgG; one only C3 | Unknown D+1 | One with CLL None | Steroids Steroids + plasma exchange | |
| Woldie et al [19] | 1 M | 24 | 7.5, nadir = 5.8 | Positive IgG + C3 | D+1 | History of AIHAi | Prednisone + cyclophosphamide | D+13 |
| Zagorski et al [20] | 1 F | 46 | 5.3 | Positive IgG + C3d | D+1 | History of ITP in pregnancy (unlikely contributing) | Died before treatment | NA |
| Vital signs | Findings |
|---|---|
| Temperature | 36.6 °C |
| Blood pressure | 160/82 mm Hg |
| Heart rate | 84 beats per minute |
| Respiratory rate | 18 breaths per minute |
| Oxygen saturation | 96% on room air |
| Physical exam | Anicteric sclera, no palpable lymphadenopathy or splenomegaly. Rectal exam guaiac negative. |
| Laboratory test | Result | Reference range (if applicable) |
|---|---|---|
| G6PD: glucose-6-phosphate dehydrogenase; IgG: immunoglobulin G; Hgb: hemoglobin. | ||
| Hemoglobin | 6.7 g/dL | 12.9 - 16.1 |
| Mean corpuscular volume | 82 fL | 79.0 - 92.2 |
| White blood cell count | 18,000/µL, 70% neutrophils | 4,200 - 9,100 |
| Platelet count | 389,000/µL | 150,000 - 400,000 |
| Lactate dehydrogenase | 2,569 U/L | 140 - 271 |
| Haptoglobin | 4 mg/dL | 32 - 197 |
| Total bilirubin | 2.7 mg/dL | 0.3 - 1.9 |
| Direct | 0.84 mg/dL | ≤ 0.18 |
| Indirect | 1.86 mg/dL | 0.1 - 1.0 |
| Absolute reticulocyte count | 71,000/µL | 26,000 - 95,000 |
| Indirect antiglobulin test | Positive, no alloantibody identified | - |
| Direct antiglobulin test | - | |
| On admission | Positive, negative IgG and weakly positive complement C3 | |
| On day 3 of hospitalization | Positive, positive IgG (2+) and positive complement C3 (3+) | |
| Eluate | Non-reactive | - |
| Cold agglutinins titer | < 1:32 | - |
| Iron | 83 µg/dL | 50 - 212 |
| Ferritin | 1,076 ng/mL | 24 - 336 |
| Vitamin B12 | > 2,800 pg/mL | 180 - 914 |
| Folate | > 20 ng/mL | ≥ 5.9 |
| G6PD | 2.2 - 5.0 U/g Hgb | 7.9 - 16.3 |
| C-reactive protein | 117 mg/L | ≤ 10.0 |
| Fibrinogen | 787 mg/dL | 200 - 393 |
| D-dimer | > 5,000 ng/mL | ≤ 574 |
| Creatinine | 0.70 - 1.30 | |
| On admission | 5.56 mg/dL | |
| On day 45 | 1.15 mg/dL | |
| Serum protein electrophoresis | Negative | |
| Diagnostic test | Findings |
|---|---|
| SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; RBC: red blood cell. | |
| Peripheral blood smear | Few echinocytes, rare schistocytes (1 - 2 per high powered field), large platelets with few platelet clumps; no significant agglutination. No immature white blood cells, frequent bands. |
| Chest X-ray | Bilateral airspace opacities consistent with SARS-CoV-2 infection |
| CT chest of abdomen and pelvis | No acute findings, negative for splenomegaly, hepatomegaly or lymphadenopathy |
| Renal studies | |
| Urinalysis | Large blood but only 3 RBCs |
| Urine microscopy | Muddy brown casts |
| Renal ultrasound | No hydronephrosis - 10.7 cm, 11.1 cm kidney size |
| Bone marrow biopsy and aspiration | Mildly hypo-cellular marrow (20-30%) with no dysplasia or abnormal hematolymphoid cell populations |