| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 11, Number 5, October 2022, pages 190-195
Hemoglobin Alpha Chain Variant Zara Associated With Familial Asymptomatic Hypoxemia
Anthony Pasquarellaa, Erin Millera, Edward C.C. Wongb, Masamichi Itob, Marc J. Braunsteina, c
aDivision of Oncology-Hematology, Department of Medicine, NYU Long Island School of Medicine, NYU Perlmutter Cancer Center, Mineola, NY, USA
bQuest Diagnostics, Secaucus, NJ, USA
cCorresponding Author: Marc J. Braunstein, Division of Oncology-Hematology, Department of Medicine, NYU Long Island School of Medicine, NYU Perlmutter Cancer Center, Mineola, NY 11051, USA
Manuscript submitted August 6, 2022, accepted October 20, 2022, published online October 31, 2022
Short title: Hb Zara With Familial Asymptomatic Hypoxemia
doi: https://doi.org/10.14740/jh1028
| Abstract | ▴Top |
Numerous hemoglobin (Hb) gene mutations have been identified, leading to a spectrum of phenotypes ranging from asymptomatic carrier states to complicated hemolytic anemias. We report a rare case of asymptomatic hypoxemia in a father and his teenage daughter both of whom were found to be carriers of Hb gene variant Zara. Workup for alternative cardiovascular causes of hypoxemia was unremarkable. Further sequencing of the alpha globin locus showed both individuals to be heterozygous for the Hb Zara c.274C>A (p.Leu92Ile) variant of unknown significance in the alpha2-globin gene. This is the first documented association of this Hb variant with familial asymptomatic hypoxemia, highlighting the importance of evaluating for hemoglobinopathies in patients with reduced oxygen saturation.
Keywords: Hemoglobinopathy; Hypoxemia; Hemoglobin Zara
| Introduction | ▴Top |
Among all hemoglobinopathies, sickle cell disease and thalassemias are the most prevalent. However, numerous additional hemoglobin (Hb) genetic variants have been described, leading to a spectrum of phenotypes with varying clinical significance [1, 2]. The globin genes, located on chromosomes 16 and 11, encode the protein components of Hb that facilitate conformational changes allowing for cooperative oxygen binding to their iron-containing heme molecules [3]. Certain Hb variants within these loci are associated with higher oxygen affinity that may also be associated with erythrocytosis. Other variants are associated with low oxygen affinity states, which may be associated with clinically significant anemia due to chemical instability regarding the structure of those Hb variants [4].
In this report, we identified a Hb variant that presented in a familial pattern. Hb Zara is a documented variant (Human Genome Variation Society (HGVS) nomenclature: HBA2:c.274C>A), first described in an adult with normal hematologic parameters, which results from a missense mutation (CTT > ATT) at codon 91 in the HBA2 gene [5, 6]. Here we provide the first description of Hb Zara leading to asymptomatic hypoxemia in a father and his daughter.
| Case Report | ▴Top |
Investigations
A White Croatian male in his 30s was referred in January 2021 for hematologic evaluation of chronically reduced oxygen saturation in the range of 90-93% since childhood. He denied dyspnea with exertion or any other respiratory symptoms. Other than reduced oxygen saturation, findings on physical examination were unremarkable. He noted that his teenage daughter was being evaluated for similar findings with unclear etiology. He had no history of respiratory infections. He took no medications and never smoked. He worked in construction and denied toxic exposures and reported no family history of cardiovascular disease. Pulmonary studies revealed a normal arterial oxygen level and normal chest imaging. Both daytime and nighttime hypoxemia was noted on a sleep study. Electrocardiography findings were normal, and echocardiogram identified an uncomplicated bicuspid aortic valve with normal ejection fraction. Initial hematologic evaluation showed a borderline reduced Hb and red blood cell count (Table 1), with normal metabolic function, including serum lactate. Further evaluation included capillary zone electrophoresis (Capillarys 2 Flexing Piercing, Sebia Lisses, France), which showed increased variant Hb (Table 1, Fig. 1a).
 Click to view | Table 1. Pertinent Laboratory Findings in the Father and Daughter Described in This Case |
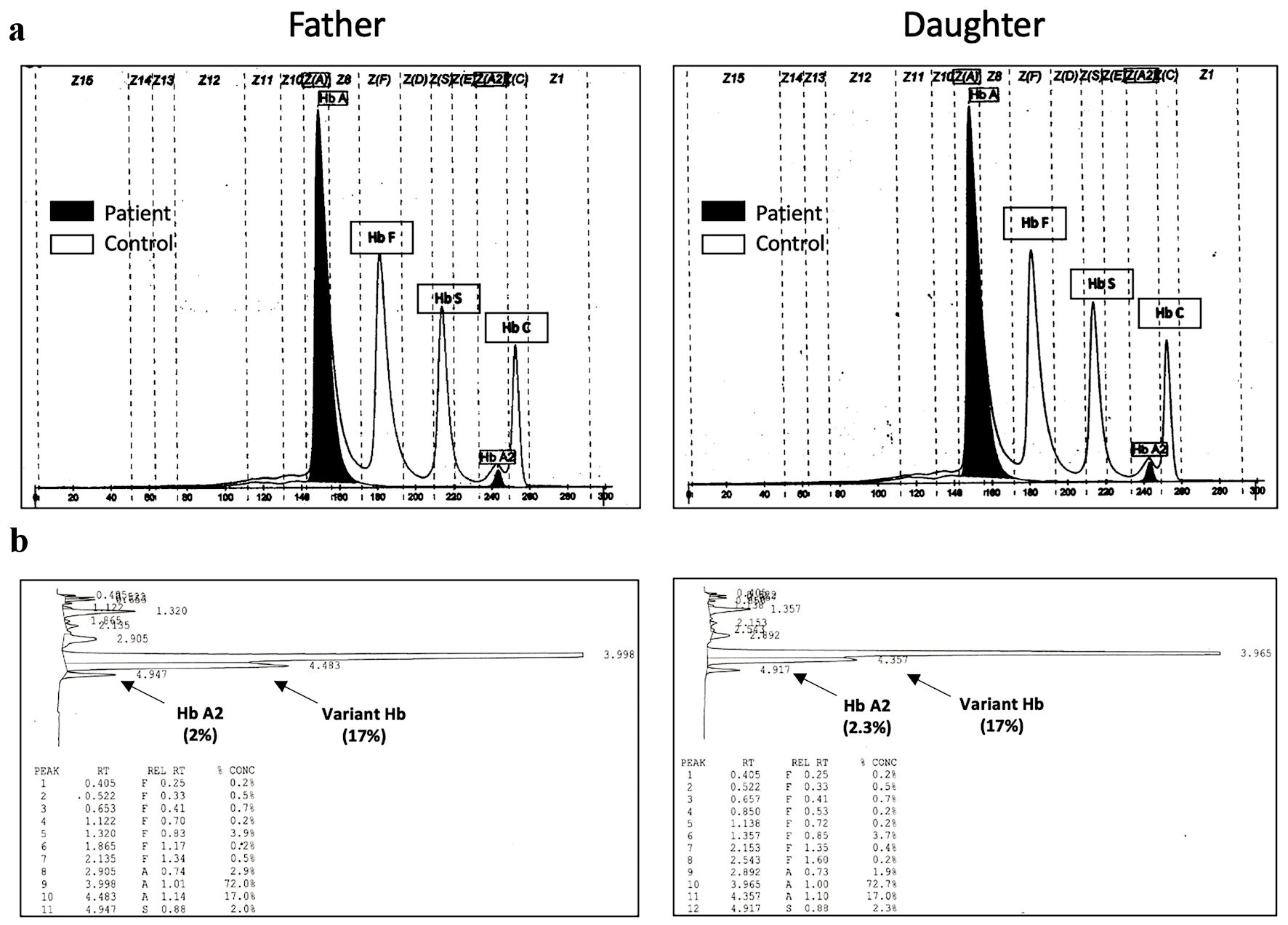 Click for large image | Figure 1. Hemoglobin (a) capillary zone electrophoresis and (b) HPLC results in the father and daughter described in this case, demonstrating an increase in variant fractions resolved on HPLC. HPLC: high-performance liquid chromatography. |
Diagnosis
To better resolve the variant Hb on capillary zone electrophoresis (Fig. 2a) [7], cation-exchange high-performance liquid chromatography (HPLC) (Trinity Ultra2 HPLC, Trinity Biotech, Wicklow, Ireland) (Fig. 1b) and alpha globin mutation testing were performed (Fig. 2). For alpha gene sequencing, the entire alpha1 and alpha2 globin genes were amplified separately by polymerase chain reaction, using gene specific primers. Dye terminator cycle sequencing was performed with six primers common to the alpha globin genes. The products of the sequencing reactions were then analyzed by capillary electrophoresis in an ABI 3730 Genetic Analyzer (SeqGen Inc., Torrance CA). The sequence data were analyzed using the ABI SeqScape™ program, v2.0 or higher (Applied Biosystems™, Waltham MA).
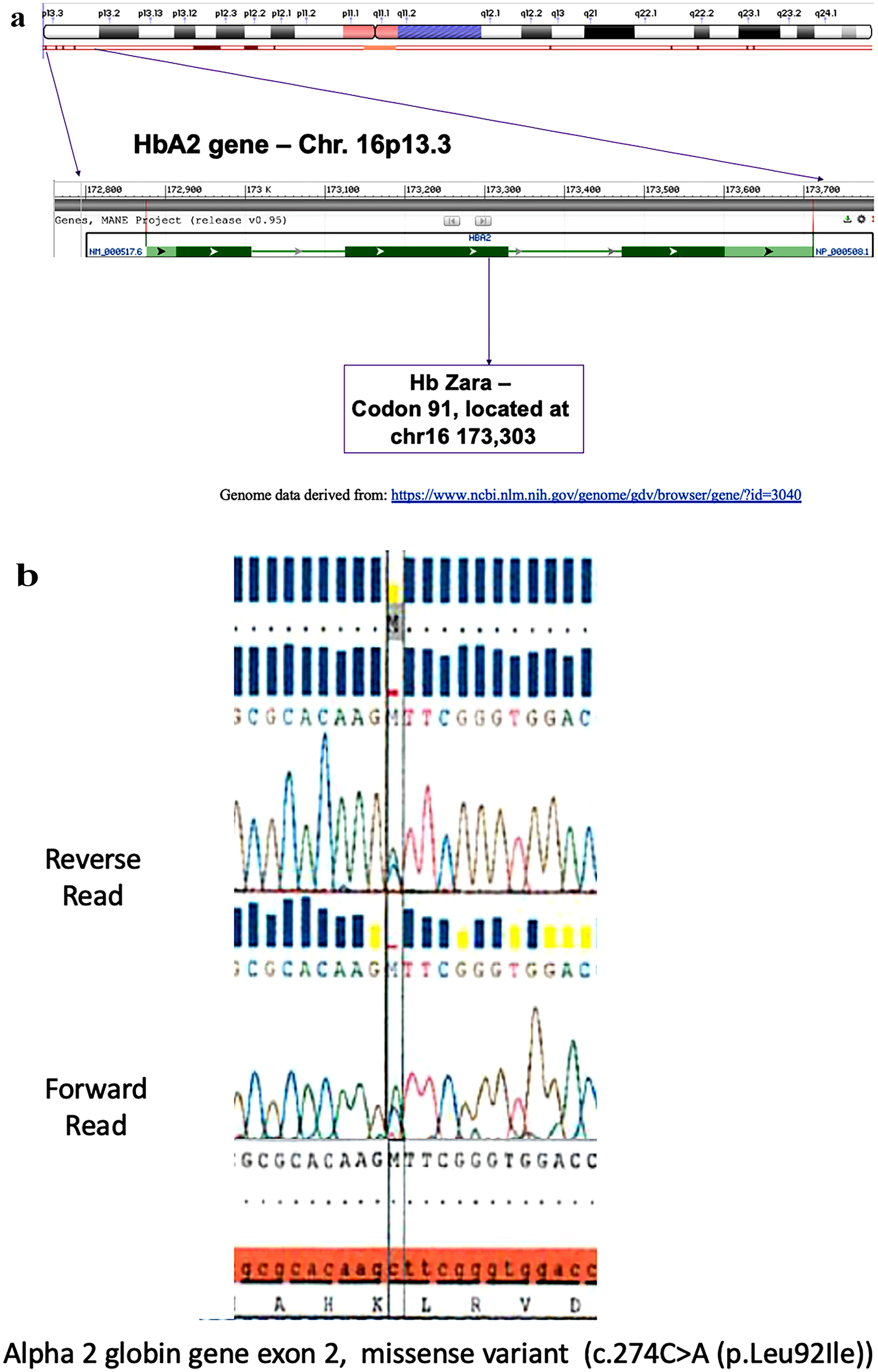 Click for large image | Figure 2. (a) Locations of Hb Zara within the HbA2 locus on the short arm of chromosome 16 [7]. (b) Representative DNA sequencing of the alpha 2 globin gene exon 2 locus. Vertical blue bars represent stronger probability, while the yellow bars represent weaker probability of results. The dark red horizontal lines indicate no match where the mutation is, which indicates a C>A missense mutation. Hb: hemoglobin. |
The patient was found to be heterozygous for the Hb Zara c.274C>A (p.Leu92Ile) variant in the HBA2 gene (Fig. 2b). Since his daughter had similar clinical findings and was anemic, we obtained consent to test her as well (Table 1). She was also found to have reduced HbA (80.6%) and increased variant Hb (17%) (Table 1), with identical pattern on electrophoresis (Fig. 1) and sequencing (Fig. 2) [7]. Both the father and his daughter did not have evidence of other causes of anemia such as nutritional deficiencies or red blood cell hemolysis, including normal lactate dehydration, haptoglobin, and total bilirubin. Hemoglobin P50 was calculated indirectly from arterial blood gas using the Doyle equation: P50n = (PaO2n/SaO2) - PaO2n, where n = 2.711 derived from the Hill equation, assuming a normal P50 of 26.6 mm Hg [8]. For the father, this was calculated to be increased 38.5 mm Hg (PaO2 100%, SaO2 93%), suggesting a right-shift associated with reduced hemoglobin oxygen affinity.
Treatment
The evaluations described above did not reveal alternative explanations for their chronic hypoxemia. Since they were both asymptomatic, without limitations in physical activity, no interventions were required. The father in this case was suggested to start continuous positive airway pressure for mild sleep apnea.
Follow-up and outcomes
On follow-up 1 year later, he and his daughter remained asymptomatic, with no new clinical findings.
| Discussion | ▴Top |
The differential diagnosis of chronic hypoxemia is broad and includes hemoglobinopathies that affect the affinity of Hb for oxygen [9]. Other conditions that can also cause chronic hypoxemia with varying symptomatology include diseases that lead to hypoventilation, such as neuromuscular disorders; ventilation-perfusion mismatch, such as with chronic lung disease (e.g., interstitial lung disease); right-to-left shunting potentially due to congenital heart malformations; and impaired oxygen diffusion capacity from alveoli to blood, as occurs with pulmonary fibrosis. These processes may occur in hematologic conditions, including hemoglobinopathies such as sickle cell disease [10].
Hemoglobinopathies are exceedingly common, especially among carriers, who tend to have a silent clinical course [11]. Many Hb variants have certain geographic associations. For example, Hb Zara has been reported as a heterozygous variant in a Croatian male, similar to the individual described in this case [12]. Hb Zara is not well characterized in the literature and has never been published as contributing to low oxygen affinity states. Our case is the first report of heterozygosity for Hb Zara, a rare hemoglobin variant, in association with asymptomatic hypoxemia. Interestingly, this Hb variant is caused by a point/missense mutation on chromosome 16, resulting in an alteration from CTT > ATT at codon 91 in alpha2 (Hb Zara) [13]. Of note, Hb Santa Barnabas, another HBA2 variant, was being considered since it can appear similarly at the locus of Hb Zara on the hemoglobin electrophoresis methods that we used. Thus, genetic testing adds an important next step in deciphering similar variants that can be indistinguishable on capillary zone electrophoresis and HPLC.
Certain hemoglobin variants are associated with low oxygen affinity states, such as Hb Bonn, Hb Venusberg, Hb Rothschild, Hb Louisville, and Hb Grove City. Zur et al reported that patients with Hb Bonn and Hb Venusberg variants may have low oxygen saturation when measured via pulse oximetry; similar to our case, this low oxygen saturation did not correlate with hypoxemia [13, 14]. Hb Rothschild also has been described as a low oxygen affinity hemoglobin variant in a young female without any obvious cardiopulmonary disease; the authors suggested that when this is seen clinically, one should rule out a dyshemoglobin state (e.g., carboxyhemoglobinemia or methemoglobinemia) [15, 16]. Given their structural instability, some Hb variants may present with both low oxygen affinity and mild hemolytic anemia, making certain variants such as Hb Louisville more clinically relevant [17]. There was no evidence of hemolytic anemia in the individuals we described in this case. However, Hb Grove City (a beta chain Hb variant) was described in a woman and her daughter who both presented with hypoxemia and mild anemia, somewhat similar to our case [18].
The pathophysiology of reduce oxygen saturation in hemoglobinopathies primarily results from low affinity of variant Hb molecules for oxygen [19]. As a tetramer, Hb normally contains two alpha and two beta subunits that cooperatively bind oxygen leading to a sigmoidal oxygen dissociation curve that can shift due to metabolic changes such as carbon dioxide levels or change in pH, commonly known as the Bohr effect [20]. Alterations in Hb subunit structure may affect oxygen binding, such as that individuals may develop high or low oxygen affinity states, leading to left or right shifts in the dissociation curve, respectively [21]. For example, in sickle cell disease, a low oxygen affinity state, chronic hypoxemia can lead to tissue damage in part due to reduced oxygen delivery [22]. In the case we describe here, there appeared to be a right shift based on the P50 calculation, suggesting decreased oxygen affinity. As over 70 low-affinity Hb variants have been described [6], it is important to perform a focused diagnostic approach to determine the clinical relevance of a particular variant [22].
This case presents an unusual co-occurrence of a Hb variants at the alpha Hb locus on chromosome 16. Both the father and his daughter in this case were noted to have chronic asymptomatic hypoxemia and without apparent organ compromise, such as pulmonary hypertension [23]. Although there are no screening guidelines for non-sickling hemoglobinopathies [24], given the rarity of Hb Zara and the benign clinical phenotype, it seems unnecessary that they be included in standard genetic screening tests. Nevertheless, this case illustrates the importance of including hemoglobinopathies in the differential during the workup for hypoxemia, particularly in patients with mild anemia, to avoid excessive and/or invasive cardiopulmonary testing.
Learning points
It is important to include hemoglobinopathies on the list of possibilities in the workup of chronic hypoxemia. This is especially true if more than one family member presents with similar clinical findings. Given the many Hb variants, workup for a suspected hemoglobinopathy should include Hb HPLC as well as alpha-globin gene sequencing if warranted based on abnormal results of these test.
Acknowledgments
None to declare.
Financial Disclosure
No funding was obtained from an external source.
Conflict of Interest
The authors report no conflicts of interest. MB has received honoraria from Abbvie, Adaptive, ADC Therapeutics, Bristol Myers Squibb, Epizyme, GlaxoSmithKline, Janssen, Pfizer, TG Therapeutics.
Informed Consent
Informed consent was obtained for both the patient and his daughter.
Author Contributions
AP and MB wrote the initial manuscript draft. AP, EM, and MB saw and managed the patients. EW and MI performed laboratory analyses. All authors contributed to the revision of the manuscript and approved the final version.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
Hb: hemoglobin; HGVS: Human Genome Variation Society; HPLC: high-performance liquid chromatography
| References | ▴Top |
- Thom CS, Dickson CF, Gell DA, Weiss MJ. Hemoglobin variants: biochemical properties and clinical correlates. Cold Spring Harb Perspect Med. 2013;3(3):a011858.
doi pubmed - Goonasekera HW, Paththinige CS, Dissanayake VHW. Population Screening for Hemoglobinopathies. Annu Rev Genomics Hum Genet. 2018;19:355-380.
doi pubmed - Bain BJ, Wild B, Stephens A, Phelan L. Variant haemoglobins: a guide to identification. Singapore: Wiley-Blackwell. 2010.
doi - Jones RT, Shih TB. Hemoglobin variants with altered oxygen affinity. Hemoglobin. 1980;4(3-4):243-261.
doi pubmed - Giardine B, Borg J, Viennas E, Pavlidis C, Moradkhani K, Joly P, Bartsakoulia M, et al. Updates of the HbVar database of human hemoglobin variants and thalassemia mutations. Nucleic Acids Res. 2014;42(Database issue):D1063-D1069.
doi pubmed - Giardine BM, Joly P, Pissard S, Wajcman H, DH KC, Hardison RC, Patrinos GP. Clinically relevant updates of the HbVar database of human hemoglobin variants and thalassemia mutations. Nucleic Acids Res. 2021;49(D1):D1192-D1196.
doi pubmed - https://www.ncbi.nlm.nih.gov/genome/gdv/browser/gene/?id=3040.
- Doyle DJ. A simple method to calculate P50 from a single blood sample. Int J Clin Monit Comput. 1997;14(2):109-111.
doi pubmed - Machogu EM, Machado RF. How I treat hypoxia in adults with hemoglobinopathies and hemolytic disorders. Blood. 2018;132(17):1770-1780.
doi pubmed - Vij R, Machado RF. Pulmonary complications of hemoglobinopathies. Chest. 2010;138(4):973-983.
doi pubmed - Lafferty JD, Waye JS, Chui DH, Crawford L, Raby A, Richardson H, Quality Management Program-Laboratory Services Hematology C. Good practice guidelines for laboratory investigation of hemoglobinopathies. Lab Hematol. 2003;9(4):237-245.
- Trova S, Mereu P, Decandia L, Cocco E, Masala B, Manca L, Pirastru M. A novel heme pocket hemoglobin variant associated with normal hematology: Hb Zara or alpha91(FG3)Leu—>Ile (alpha2) (HBA2: c.274C > A). Hemoglobin. 2015;39(6):427-429.
doi pubmed - Zur B, Hornung A, Breuer J, Doll U, Bernhardt C, Ludwig M, Stoffel-Wagner B. A novel hemoglobin, Bonn, causes falsely decreased oxygen saturation measurements in pulse oximetry. Clin Chem. 2008;54(3):594-596.
doi pubmed - Zur B, Bagci S, Ludwig M, Stoffel-Wagner B. Oxygen saturation in pulse oximetry in hemoglobin anomalies. Klin Padiatr. 2012;224(4):259-265.
doi pubmed - Alli NA, Wessels P, Rampersad N, Clark BE, Thein SL. Detection of Hb Rothschild HBB: c.[112T>A or 112T>C], through high index of suspicion on abnormal pulse oximetry. Hemoglobin. 2017;41(2):137-139.
doi pubmed - Hladik A, Lynshue K. Dyshemoglobinemias and pulse oximetry: a therapeutic challenge. J Pediatr Hematol Oncol. 2008;30(11):850-852.
doi pubmed - Jung J, Garnett E, Vispo B, Chen X, Cao J, Tarek Elghetany M, Devaraj S. Misidentification of unstable, low oxygen affinity hemoglobin variant. Clin Chim Acta. 2020;509:177-179.
doi pubmed - Taliercio RM, Ashton RW, Horwitz L, Swanson KC, Wendt PC, Hoyer JD, Oliveira JL. Hb Grove City [beta38(C4)Thr—>Ser, ACC>AGC; HBB: c.116C>G]: a new low oxygen affinity beta chain variant. Hemoglobin. 2013;37(4):396-403.
doi pubmed - Yudin J, Verhovsek M. How we diagnose and manage altered oxygen affinity hemoglobin variants. Am J Hematol. 2019;94(5):597-603.
doi pubmed - Malte H, Lykkeboe G, Wang T. The magnitude of the Bohr effect profoundly influences the shape and position of the blood oxygen equilibrium curve. Comp Biochem Physiol A Mol Integr Physiol. 2021;254:110880.
doi pubmed - Murray JF, Mason RJ. Murray and Nadel's textbook of respiratory medicine, Chapter 94: Pulmonary Complications of Hematologic Diseases, 6th Edition. Philadelphia, PA: Saunders/Elsevier. 2016.
- Kutlar F. Diagnostic approach to hemoglobinopathies. Hemoglobin. 2007;31(2):243-250.
doi pubmed - West JB. Physiological effects of chronic hypoxia. N Engl J Med. 2017;376(20):1965-1971.
doi pubmed - Angastiniotis M, Eleftheriou A, Galanello R, Harteveld CL, Petrou M, Traeger-Synodinos J, Giordano P, et al. In: Old J, eds. Prevention of thalassaemias and other haemoglobin disorders: Volume 1: Principles. Nicosia (Cyprus), 2013.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


