| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 12, Number 6, December 2023, pages 283-286
Extensive Intracardiac Cement Embolism in a Patient Undergoing Workup for Bone Marrow Transplant
Gavisha Waidyaratnea, d , Caitlin Bennettb, Elvira Umyarovac, Naresh Bummac
aDepartment of Internal Medicine, The Ohio State University Wexner Medical Center, Columbus, OH 43210, USA
bDepartment of Hospice and Palliative Medicine, Yale School of Medicine, New Haven, CT 06510, USA
cDivision of Hematology and Oncology, The Ohio State University Wexner Medical Center, Columbus, OH 43210, USA
dCorresponding Author: Gavisha Waidyaratne, Department of Internal Medicine, The Ohio State University Wexner Medical Center, Columbus, OH 43210, USA
Manuscript submitted October 5, 2023, accepted November 25, 2023, published online December 9, 2023
Short title: Cement Embolus in a Patient Evaluated for BMT
doi: https://doi.org/10.14740/jh1202
| Abstract | ▴Top |
Cement emboli are a well-established complication of kyphoplasties and vertebroplasties and can easily be mistaken for wires. While kyphoplasties are commonly performed for vertebral fractures caused by metastases from malignancies such as multiple myeloma, the implication of cement emboli in bone marrow transplant (BMT) patients is not well documented. Our patient presented with an incidental intracardiac cement embolism found while undergoing workup for BMT. He was managed conservatively, but transplant workup was put on hold until the embolism could be removed due to the risks associated with cement emboli. The significance of cement emboli in immunocompromised patients needs to be further investigated.
Keywords: Cement embolism; Stem cell transplantation; Multiple myeloma; Transplant; Kyphoplasty
| Introduction | ▴Top |
Intracardiac and intrapulmonary cement emboli are well-known complications of percutaneous kyphoplasty, a procedure which stabilizes vertebral compression fractures with the injection of bone cement into the vertebral body [1]. This procedure is helpful in the management of painful pathologic fractures caused by invasive malignancies such as breast cancer, lung cancer, prostate cancer, and multiple myeloma [2]. While largely safe and minimally invasive, the leakage of cement into the paravertebral veins, azygous venous system, or vena cava with subsequent migration into the pulmonary arterial system is a major complication [3]. Symptomatic intracardiac cement emboli are an even less commonly documented complication, with a reported incidence of 0.3% [3, 4]. The risks of developing a cement embolism include the utilization of low/medium viscosity poly(methyl methacrylate) (PMMA), treatment of multiple levels in one session, and lesions in the thoracic vertebra [1, 3]. While most intracardiac cement emboli are asymptomatic, complications can vary from mild symptoms to death [1, 3, 5]. Surprisingly there appears to be only one other documented case report of a cement embolism occurring in an individual undergoing bone marrow transplant (BMT) [5]. Our report aims to explore the case of an extensive intracardiac cement embolism in a patient undergoing workup for BMT and reflect on how cement emboli may affect BMT evaluation.
| Case Report | ▴Top |
Investigations
A 64-year-old man with a history of sarcoidosis and multiple myeloma status-post induction therapy with daratumumab, bortezomib, lenalidomide, and dexamethasone (DVRd) presented for investigation of a foreign body (FB) that was incidentally visualized on echocardiogram during stem cell transplant (BMT) workup. Despite no prior history of central line placement or cardiac catheterization, the echo noted a linear density concerning for a wire in the inferior vena cava (IVC) and extending into the right atrium (RA) and right ventricle (RV). He did however have multiple kyphoplasties of the thoracic and lumbar spine in the months preceding presentation. He most recently underwent an uncomplicated kyphoplasty of T6 and T10 6 weeks prior to presentation. On evaluation, the patient was asymptomatic and his exam was unremarkable.
Diagnosis
Chest computed tomography (CT) confirmed a retained FB in the IVC extending superiorly into the RA and proximal RV (Fig. 1). A positron emission tomography (PET) scan also visualized the FB originating from L2-3 and travelling into the IVC (Fig. 2). Given that the patient was asymptomatic, cardiac surgery did not recommend acute surgical intervention and advised discussing endovascular retrieval options with interventional radiology (IR).
 Click for large image | Figure 1. Chest computed tomography without contrast with cement embolism (arrow) seen in right atrium and right ventricle. |
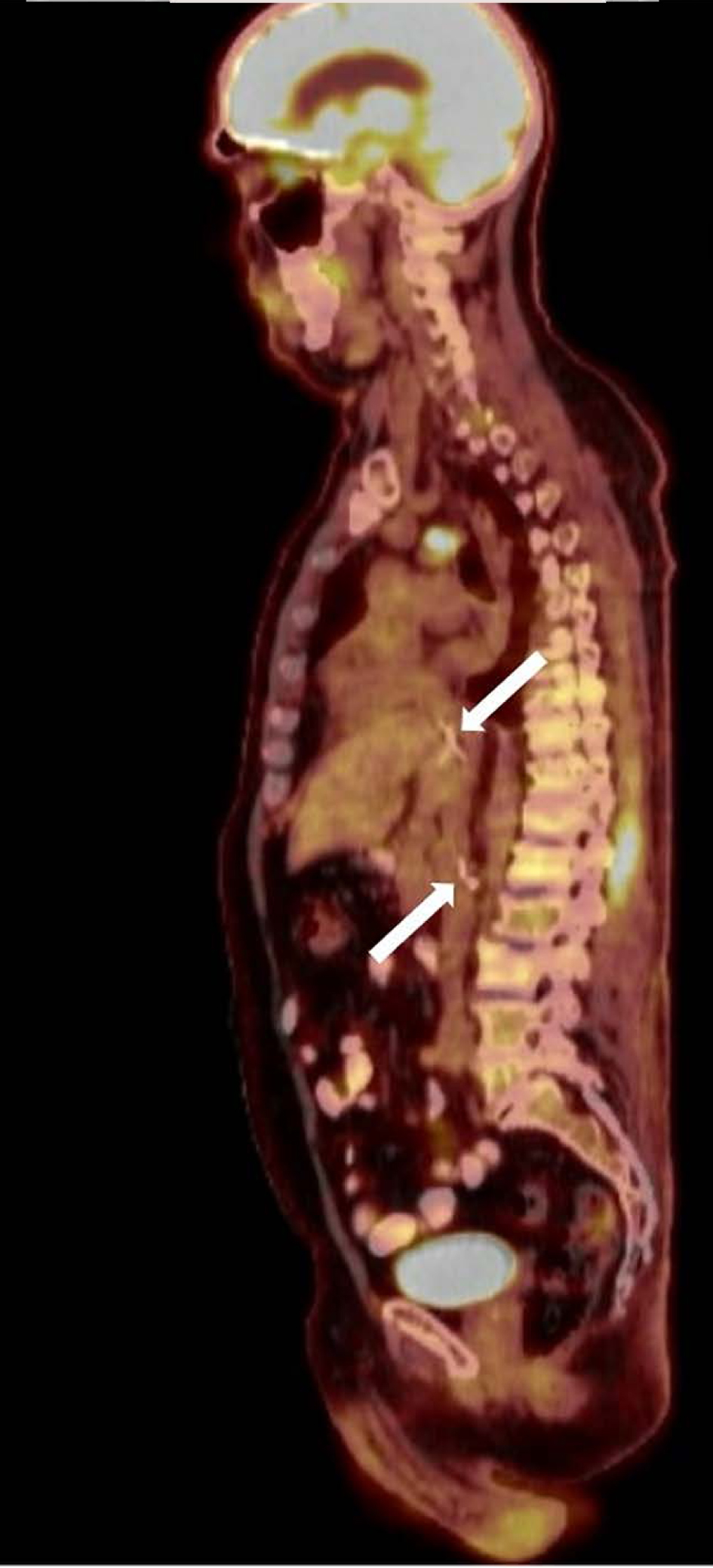 Click for large image | Figure 2. Positron emission tomography in coronal plane with cement embolism (arrows) originating around L2-L3 and extending up inferior vena cava. |
Treatment
IR reviewed the available imaging and confirmed that the FB was likely a cement embolism from prior kyphoplasty, with the caudal aspect of cement tethered to the lumbar vein. IR recommended IVC venography with cement retrieval and possible deployment of a temporary embolic protection device. Risks of not proceeding with retrieval were discussed including cement ingratiation, thromboemboli, or cardiac/venous injury. After discussion with family, the patient elected to forego the procedure and was discharged. The patient’s case was discussed at tumor board, and the BMT committee recommended that transplant workup be put on hold until the cement embolus could be removed.
Follow-up and outcomes
The patient sought a second opinion at another institution and was recommended against proceeding with BMT due to the risks involved with the cement embolism. He completed a fifth cycle of DVRd and was then started on single agent lenalidomide with the later addition of daratumumab for maintenance therapy. One year later, he continued to remain asymptomatic with regards to his embolism, with evidence of stable multiple myeloma on biopsy and laboratory testing. Follow-up PET scan at this time confirmed stable bony involvement of his multiple myeloma and no major changes to the cement embolism.
| Discussion | ▴Top |
The incidence of cement emboli is high, with rates of pulmonary cement emboli varying from 4.6% to 26.9%. There have been multiple case reports of intracardiac emboli involving the right side of the heart [3]. In addition, cement emboli are easily mistaken for wires or other FB on imaging [1]. A detailed history and further imaging are necessary to accurately diagnose a cement embolism. Though most cement emboli are asymptomatic, complications include tamponade, valvular damage, cardiac perforation, and death [1, 3]. Management strategies include conservative management, anticoagulation, percutaneous retrieval, and cardiac surgery. Invasive options can have risks such as cement breakage or damage of the intima after endovascular manipulation [6, 7]. In cases of small asymptomatic cement emboli, previous studies have shown that patients who received conservative management continued to remain asymptomatic at long-term follow-up [8]. Anticoagulation, such as heparin, enoxaparin, warfarin, and direct oral anticoagulants (DOACs), has been reported in various case reports as another non-invasive strategy for management [9, 10]. However, the evidence behind the use of anticoagulation for cement emboli is lacking, and this option is accompanied by an increased risk of bleeding [11].
Despite the extent of published studies on cement emboli, there is limited guidance on how to approach this complication in the setting of an immunocompromised patient. We present the unique case of a large, asymptomatic intracardiac cement embolism in a patient with multiple myeloma undergoing evaluation for BMT. Studies have suggested that the incidence of cement embolism is higher in multiple myeloma compared to other malignancies; this may be related to the frequency with which myeloma patients undergo treatment for vertebral body fractures [12, 13]. Some also suggest that cement leakage is more expected in malignancy compared to osteoporosis, possibly due to neo-angiogenesis [14]. Unfortunately, the data on cement emboli in patients with BMT or solid organ transplant are scarce and limited to several case reports [1, 4]. BMT patients are already at high risk of infection, cardiotoxicity, and bleeding. Furthermore, some cancer therapies such as lenalidomide further increase thrombotic risk [15]. Therefore, it is difficult to assess how the risk of complication from cement emboli should be weighed in a patient undergoing BMT evaluation. We recommend an individualized and multidisciplinary approach to these patients that considers the extent of the embolism, symptoms, and comorbidities. While our patient did not suffer any immediate complications from the cement embolus, our case is limited by its recency. Additionally for our patient, the significance of a cement embolus precluding the therapeutic opportunity of BMT should be acknowledged as a potential major consequence of this complication. This case suggests that while cement emboli may not be an absolute contraindication to BMT, the long-term implications are not clear.
Learning points
Cement emboli are an important complication of kyphoplasty that can be easily mistaken for FB and have major risks. A multidisciplinary team approach is crucial for diagnosis and management, but the data around various management strategies are mixed. The long-term significance of these risks in immunocompromised patients such as those undergoing BMT, is even less clear and requires further investigation.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
All authors participated in the care of the patient. GW participated in the conceptualization and writing of the manuscript. All authors contributed to the revisions and final approval of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study is available within the article.
Abbreviations
BMT: bone marrow transplant; CT: computed tomography; DOAC: direct oral anticoagulant; DVRd: daratumumab, bortezomib, lenalidomide, and dexamethasone; FB: foreign body; IR: interventional radiology; IVC: inferior vena cava; PET: positron emission tomography; PMMA: poly(methyl methacrylate); RA: right atrium; RV: right ventricle
| References | ▴Top |
- Shridhar P, Chen Y, Khalil R, Plakseychuk A, Cho SK, Tillman B, Kumta PN, et al. A review of PMMA bone cement and intra-cardiac embolism. Materials (Basel). 2016;9(10):821.
doi pubmed pmc - Hariri O, Takayanagi A, Miulli DE, Siddiqi J, Vrionis F. Minimally invasive surgical techniques for management of painful metastatic and primary spinal tumors. Cureus. 2017;9(3):e1114.
doi pubmed pmc - Fadili Hassani S, Cormier E, Shotar E, Drir M, Spano JP, Morardet L, Collet JP, et al. Intracardiac cement embolism during percutaneous vertebroplasty: incidence, risk factors and clinical management. Eur Radiol. 2019;29(2):663-673.
doi pubmed - Pan HY, Wu TY, Chen HY, Wu JY, Liao MT. Intracardiac cement embolism: images and endovascular treatment. Circ Cardiovasc Imaging. 2021;14(4):e011849.
doi pubmed - Siddiqui AS, Goodarzi A, Majumdar T, Kaleekal T. A rare case of pulmonary cement embolism in a lung transplant patient. Respir Med Case Rep. 2018;24:63-64.
doi pubmed pmc - MacTaggart JN, Pipinos, II, Johanning JM, Lynch TG. Acrylic cement pulmonary embolus masquerading as an embolized central venous catheter fragment. J Vasc Surg. 2006;43(1):180-183.
doi pubmed - Bassawon R, Sirajuddin S, Martucci G, Shum-Tim D. Snare or scalpel: challenges of intracardiac cement embolism retrieval. Ann Thorac Surg. 2022;113(2):e107-e110.
doi pubmed - Anselmetti GC, Manca A, Montemurro F, Hirsch J, Chiara G, Grignani G, Carnevale Schianca F, et al. Percutaneous vertebroplasty in multiple myeloma: prospective long-term follow-up in 106 consecutive patients. Cardiovasc Intervent Radiol. 2012;35(1):139-145.
doi pubmed - Geraci G, Lo Iacono G, Lo Nigro C, Cannizzaro F, Cajozzo M, Modica G. Asymptomatic bone cement pulmonary embolism after vertebroplasty: case report and literature review. Case Rep Surg. 2013;2013:591432.
doi pubmed pmc - Rahimizadeh A, Hassani V, Soufiani H, Rahimizadeh A, Karimi M, Asgari N. Symptomatic pulmonary cement embolism after pedicle screw polymethylmethacrylate cement augmentation: A case report and review. Surg Neurol Int. 2020;11:18.
doi pubmed pmc - Waler AR, Sanchez KJ, Parikh AA, Okorie ON. A case of pulmonary cement embolism managed through symptomatic treatment. Case Rep Crit Care. 2020;2020:2425973.
doi pubmed pmc - Mansour A, Abdel-Razeq N, Abuali H, Makoseh M, Shaikh-Salem N, Abushalha K, Salah S. Cement pulmonary embolism as a complication of percutaneous vertebroplasty in cancer patients. Cancer Imaging. 2018;18(1):5.
doi pubmed pmc - Choe DH, Marom EM, Ahrar K, Truong MT, Madewell JE. Pulmonary embolism of polymethyl methacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am J Roentgenol. 2004;183(4):1097-1102.
doi pubmed - Patel Z, Sangani R, Lombard C. Cement pulmonary embolism after percutaneous kyphoplasty: An unusual culprit for non-thrombotic pulmonary embolism. Radiol Case Rep. 2021;16(11):3520-3525.
doi pubmed pmc - Debbie Jiang MD, Alfred Ian Lee MD. Thrombotic risk from chemotherapy and other cancer therapies. Cancer Treat Res. 2019;179:87-101.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


