| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 3, Number 3, September 2014, pages 86-88
Prolymphocytic and Richter’s Transformation in Peripheral Blood: A Case Report and Review of Literature
Chanchal Ranaa, b, Seema Sharmaa, Mitali Agarwala
aDepartment of Pathology, Sanjay Gandhi Postgraduate Institute of Medical Science and Research, Lucknow, Uttar Pradesh, India
bCorresponding Author: Chanchal Rana, Department of Pathology, Sanjay Gandhi Postgraduate Institute of Medical Science and Research, Lucknow, Uttar Pradesh, India
Manuscript accepted for publication July 31, 2014
Short title: Prolymphocytic and Richter’s Transformation
doi: https://doi.org/10.14740/jh121w
| Abstract | ▴Top |
The indolent course of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) is occasionally altered by transformation to a histologically distinct, rapidly progressive, and clinically unresponsive hematologic malignant neoplasm, a phenomenon known as Richter’s transformation. The most likely site of transformation is enlarging lymph nodes. The malignant cells of Richter’s transformation can occasionally be seen in the bone marrow and only very rarely in the peripheral blood. We report an interesting case of CLL which underwent a full spectrum of transformation from classical CLL to prolymphocytic leukemia and finally to Richter’s transformation with an unusual feature being a leukemic Richter’s transformation, i.e. Richter’s transformation in the peripheral blood.
Keywords: Chronic lymphocytic leukemia; Prolymohocytic leukemia; Richter’s transformation; Peripheral blood
| Introduction | ▴Top |
Chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) is an indolent lymphoproliferative disorder, almost exclusively of B-cell origin, occurring in mid to late adulthood [1]. Transformation to a more aggressive and distinct hematolymphoid malignant neoplasm occurs in 25% to 50% of cases [2]. The most common is prolymphocytic transformation, an outcome in up to 15% to 30% of cases, manifested by the presence of 11% to 55% of prolymphocytes in the peripheral blood with a median survival of about 2 years [2]. Less common is transformation into a large cell lymphoma with immunoblastic features, also known as Richter syndrome (RT), a phenomenon that is seen in 2% to 9% of patients with CLL/SLL. RT pursues a much more aggressive course, with a median survival of only 4 - 5 months [3]. Disease onset is typically manifested by a sudden clinical deterioration of the patient and is characterized by rapid progression of lymphadenopathy, by extranodal disease and by constitutional symptoms.
Rare cases of transformation into leukemia, small non-cleaved cell lymphoma, Hodgkin lymphoma and multiple myeloma have also been described [4-7]. Mostly the lymphomatous clones arise in the lymph nodes but there can be extranodal involvement also. The malignant cells of RT can occasionally be seen in the bone marrow and only very rarely in the peripheral blood [3].
We are reporting a case with a well established history of CLL which transformed from a classical CLL to prolymphocytic CLL and finally underwent leukemic Richter’s transformation (in peripheral blood) followed by death shortly in a span of about 11.5 years (May 1999 - Oct 2010).
| Case Report | ▴Top |
A 64-year-old male was referred to our institute in May 1999 with complaints of fatigue and generalized weakness. On physical examination, he had bilateral cervical lymphadenopathy and splenomegaly. The lymph nodes were discrete, non-tender, freely movable and 1 - 2 cm in greatest dimension. He was diagnosed as a case of CLL on peripheral blood examination which showed 92% of small sized lymphocytes with clumped chromatin, in conspicuous nucleoli with small rim of cytoplasm along with presence of many smudge/basket cells in the background (Fig. 1). Hemogram findings showed moderate anemia (hemoglobin 9.5 g/dL), marked leucocytosis (total leucocyte count 403.5 × 106/µL), thrombocytopenia (platelet count 45,000/µL). The absolute lymphocyte count was 371.2 × 106/µL. Bone marrow aspiration and bone marrow biopsy confirmed the diagnosis of CLL. On immunophenotyping these lymphoid cells were positive for CD5, CD23 and CD19, negative for FMC-7 and CD20, and also showed mono-clonality for kappa light chain. According to Rai classification he was staged in high risk group (stage IV). The patient compliance was poor and he left the hospital without treatment.
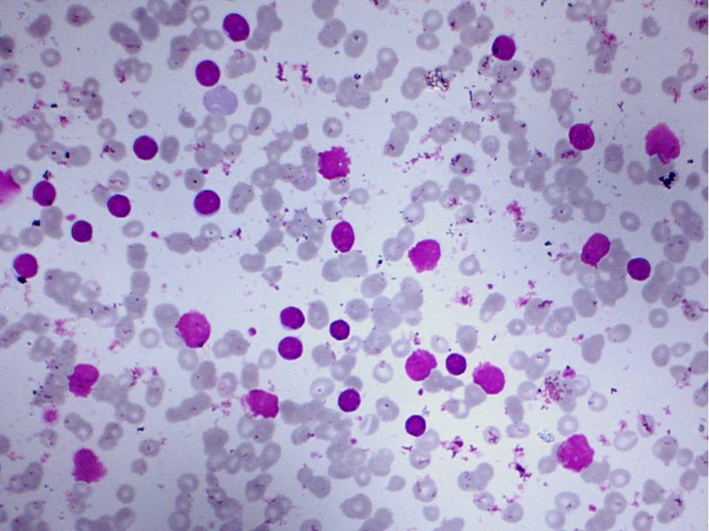 Click for large image | Figure 1. Classical chronic lymphocytic leukemia: small sized lymphoid cells with smudge cells in the background. |
He presented again in 2005 with complaints of fever, weakness and progressively increasing lymph nodes and splenomegaly. Based on his previous diagnosis of CLL he was started on combination therapy (rituximab, cyclophosphamide and dexamethasone). There was significant improvement in response after four cycles of chemotherapy but then there were features of relapse. The patient was subsequently treated with a further course of fludarabine and the monoclonal antibody (rituximab/alemtuzumab). He received on and off treatment thereafter due to poor compliance till 2008 when splenectomy was performed for reduction of disease. Histopathological examination of spleen revealed SLL/CLL. At the same time peripheral blood examination showed 26% prolymphocytes. This suggested a transformation of classical CLL to prolymphocytic leukemia.
He was again admitted in July 2010 with worsening B symptoms (fever, fatigue, weight loss, etc.) and massively enlarged cervical lymph nodes along with presence of bilateral axillary and bilateral inguinal lymph nodes. He was evaluated and peripheral blood examination showed presence of two separate populations of lymphocytes. The first were small cells with clumped chromatin, scant cytoplasm and inconspicuous nucleoli. The second were large cells with pleomorphic nuclei, open chromatin distinct nucleoli and moderate to abundant amount of cytoplasm (92%) (Fig. 2). These findings suggested the presence of leukemic Richter’s transformation. The patient died of multiorgan failure 3 months after his last admission.
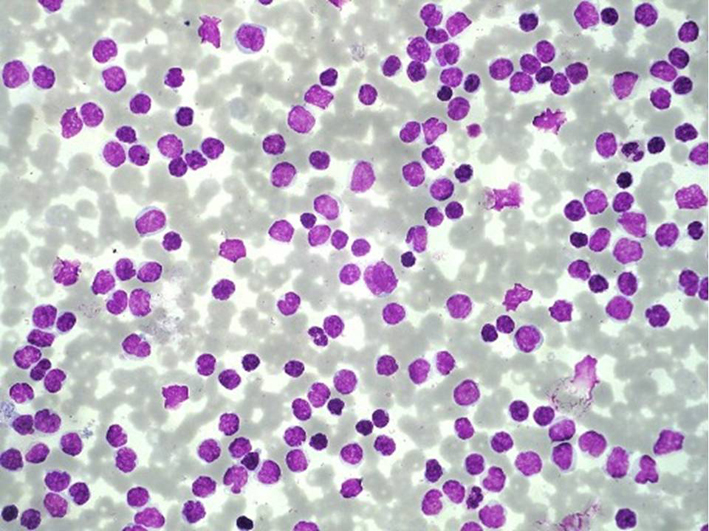 Click for large image | Figure 2. Leukemic Richter’s transformation: atypical cells with pelomorhic nuclei, dispersed chromatin, prominent nucleoli and scant cytoplasm along with interspersed lymphoid cells. |
| Discussion | ▴Top |
Richter’s transformation was first described in 1928 by Maurice Richter as the development of large cell lymphoma in the setting of underlying CLL/SLL [8]. The incidence of CLL/SLL to defuse large B-cell lymphoma has been variously estimated as 2-9% [3]. Prolymphocytic leukemia is a more frequent disease transformation [2]. Other rare transformations include multiple myeloma and acute leukemia, which usually occurs in less than 1% of CLL patients [6]. Clinical onset is heralded by progressively increasing lymphadenopathy, splenomegaly and worsening B symptoms (fever, weight loss, etc.). The lymphomatous clone in Richter’s transformation frequently arises in lymph nodes or bone marrow and disseminates to other organs. Rarely, RT may present with extranodal involvement.
Our case report is interesting as we are not only reporting a full spectrum of transformation from classical CLL to prolymphocytic leukemia and finally to leukemic Richter’s transformation but are also reporting a rare situation where the Richter’s transformation has occurred in peripheral blood.
Risk factors for development of RT are poorly defined. However some studies have tried to define these risk factors, which are elevated serum LDH, systemic symptoms, enlarging lymph nodes, monoclonal gammopathy, younger age, prior therapy, absence of deletion 13q14, CD expression, etc. [9, 10].
The diffuse large cell lymphoma clone may arise from the underlying CLL/SLL, may represent evolution from a biclonal phenotype in CLL/SLL or may represent a new clone. More recent studies have suggested that in 90 to 100% cases there is clonal evolution from underlying CLL/SLL [9, 11]. The acquisition of new genetic abnormalities is associated with progression to RT. Some common abnormalities include del 11q, del 17p, del chromosome 20, trisomy 12, etc. [9]. RT cases also show higher levels of activation-induced cytidine deaminase, mutation of c-myc, p53, PAX-5, INK4a/ARF and RhoH [12, 13]. These abnormalities may cause CLL cells to proliferate and, by facilitating the acquisition of new genetic abnormalities, to transform into RT cells. Although pathogenic role of virus is unclear, evidence for its involvement is probably greatest in Hodgkin’s lymphoma variant of RT in which Epstein-Barr virus can be found in the RT cells in majority of limited reported cases [14].
Though biopsy from a likely site of transformation, usually lymph node, is required from establishing the diagnosis, imaging like gallium and PET scan may provide guidance on choice of biopsy site [15, 16].
RT has been associated with dismal prognosis with a median survival of 4 - 5 months [3]. Our patient died of multiorgan failure within 3 months of transformation. Treatment of RT has generally relied on combination therapy as used in NHL or ALL with overall response rates ranging from 5% to 40%. No statistical significance addition of fludarabine has been associated with improvement; however, in our case, there was no such improvement [17]. Hence there is still a need for effective treatment plan for patients of RT.
| References | ▴Top |
- Johnston JB. Chronic Lymphocytic Leukemia in Wintrobe's Clinical Hematology, Lipincott Williams and Wilkins: 11th ed. 2001;2:2429-2464.
- Foucar K. Chronic lymphoproliferative disorders. In: Foucar K, ed. Bone Marrow Pathology. Chicago, Ill: ASCP Press. 1995;275-314.
- Tsimberidou AM, Keating MJ. Richter syndrome: biology, incidence, and therapeutic strategies. Cancer. 2005;103(2):216-228.
doi pubmed - Brecher M, Banks PM. Hodgkin's disease variant of Richter's syndrome. Report of eight cases. Am J Clin Pathol. 1990;93(3):333-339.
pubmed - Lee A, Skelly ME, Kingma DW, Medeiros LJ. B-cell chronic lymphocytic leukemia followed by high grade T-cell lymphoma. An unusual variant of Richter's syndrome. Am J Clin Pathol. 1995;103(3):348-352.
pubmed - Rozman C, Montserrat E. Chronic lymphocytic leukemia. N Engl J Med. 1995;333(16):1052-1057.
doi pubmed - Litz CE, Arthur DC, Gajl-Peczalska KJ, Rausch D, Copenhaver C, Coad JE, Brunning RD. Transformation of chronic lymphocytic leukemia to small non-cleaved cell lymphoma: a cytogenetic, immunological, and molecular study. Leukemia. 1991;5(11):972-978.
pubmed - Richter MN. Generalized Reticular Cell Sarcoma of Lymph Nodes Associated with Lymphatic Leukemia. Am J Pathol. 1928;4(4):285-292 287.
- Robertson LE, Pugh W, O'Brien S, Kantarjian H, Hirsch-Ginsberg C, Cork A, McLaughlin P, et al. Richter's syndrome: a report on 39 patients. J Clin Oncol. 1993;11(10):1985-1989.
pubmed - Rossi D, Cerri M, Capello D, Deambrogi C, Rossi FM, Zucchetto A, De Paoli L, et al. Biological and clinical risk factors of chronic lymphocytic leukaemia transformation to Richter syndrome. Br J Haematol. 2008;142(2):202-215.
doi pubmed - Bea S, Lopez-Guillermo A, Ribas M, Puig X, Pinyol M, Carrio A, Zamora L, et al. Genetic imbalances in progressed B-cell chronic lymphocytic leukemia and transformed large-cell lymphoma (Richter's syndrome). Am J Pathol. 2002;161(3):957-968.
doi - Smit LA, van Maldegem F, Langerak AW, van der Schoot CE, de Wit MJ, Bea S, Campo E, et al. Antigen receptors and somatic hypermutation in B-cell chronic lymphocytic leukemia with Richter's transformation. Haematologica. 2006;91(7):903-911.
pubmed - Reiniger L, Bodor C, Bognar A, Balogh Z, Csomor J, Szepesi A, Kopper L, et al. Richter's and prolymphocytic transformation of chronic lymphocytic leukemia are associated with high mRNA expression of activation-induced cytidine deaminase and aberrant somatic hypermutation. Leukemia. 2006;20(6):1089-1095.
doi pubmed - Tsimberidou AM, O'Brien S, Khouri I, Giles FJ, Kantarjian HM, Champlin R, Wen S, et al. Clinical outcomes and prognostic factors in patients with Richter's syndrome treated with chemotherapy or chemoimmunotherapy with or without stem-cell transplantation. J Clin Oncol. 2006;24(15):2343-2351.
doi pubmed - Partyka S, O'Brien S, Podoloff D, Kantarjian H, Keating MJ. The usefulness of high dose (7-10mci) gallium (67Ga) scanning to diagnose Richter's transformation. Leuk Lymphoma. 1999;36(1-2):151-155.
doi pubmed - Bruzzi JF, Macapinlac H, Tsimberidou AM, Truong MT, Keating MJ, Marom EM, Munden RF. Detection of Richter's transformation of chronic lymphocytic leukemia by PET/CT. J Nucl Med. 2006;47(8):1267-1273.
pubmed - Dabaja BS, O'Brien SM, Kantarjian HM, Cortes JE, Thomas DA, Albitar M, Schlette ES, et al. Fractionated cyclophosphamide, vincristine, liposomal daunorubicin (daunoXome), and dexamethasone (hyperCVXD) regimen in Richter's syndrome. Leuk Lymphoma. 2001;42(3):329-337.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


