| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 3, Number 3, September 2014, pages 89-90
Lennert’s Maze Game: A Diagnostic Hematological Challenge
Nilma Malika, b, Vishwanath Pattana, Waqas Jehangira, Hongxiu Luoa, Yazan Vwicha, Teena Mathewa, Shuvendu Sena, Abdalla Yousifa
aInternal Medicine Department, Raritan Bay Medical Center, 530 New Brunswick Avenue, Perth Amboy, NJ 08861, USA
bCorresponding Author: Nilma Malik, 97 Tennyson Street, Carteret, NJ 07008, USA
Manuscript accepted for publication July 25, 2014
Short title: Lennert Lymphoma
doi: https://doi.org/10.14740/jh165w
| Abstract | ▴Top |
Lennert lymphoma is a subset of peripheral T-cell lymphoma (PTCL) that constitutes about 30% of T-cell lymphomas. The immunophenotypes usually are positive for pan-antigens, such as CD2, CD3, CD5 or CD7. About half cases present aberrantly without the pan-antigens. This rare case opens up a new horizon of thought process, as it illustrates the clinical presentation of PTCL with aberrant hematological parameters. It emphasizes on diagnostic and treatment challenges of Lennert lymphoma presenting with a triad of eosinophilia, lactic acidosis and multi-organ thrombosis. Early treatment with chemotherapy rather than supportive measures is crucial as it has shown significant morbidity benefits.
Keywords: Lennert; Lactic acidosis; Eosinophilia; Thrombosis; Hemophagocytosis; Chemotherapy; Thrombomodulin; Prognosis
| Introduction | ▴Top |
The incidence of peripheral T-cell lymphomas (PTCL), not otherwise specified (NOS) has increased in USA from 0.1 cases/100,000 population in 1992 to 0.4 cases/100,000 population in 2006 [1]. We report a rare case of Lennert’s, variant of PTCL presenting with eosinophilia, multi-organ thrombosis and lactic acidosis.
| Case Report | ▴Top |
A 47-year-old male was admitted for evaluation of 4-day history of worsening shortness of breath and pain in his right hand and leg. One month prior to admission he was diagnosed with bilateral lower extremity, hepatic vein and inferior vena cava thrombosis and was started on warfarin. There was no family history of venous clots or stroke. Upon admission he had an HR 87/min, BP 125/67 mm Hg, RR 16/min, T 98.6 °F and SO2 95%. Clinical examination revealed absent right ulnar and dorsalis pedis pulses and a papular rash over trunk and arms (Fig. 1a, b). Labs were significant for Hb 7 g/dL, WBC 19,800/µL (neutrophil 82%, eosinophils 69% and metamyelocyte 1%). Platelets were 487,000/µL, glucose 120 mg/dL, BUN 39 mg/dL, ceatinine 0.8 mg/dL, bicarbonate 14 mEq/L, anion gap 22 mEq/L, lactic acid 6.1 mmol/L and INR 1.8. Urine drug screen, sepsis and hypercoagulable workup were negative. Peripheral blood smear showed anisopoikilocytosis, and no parasites were identified. CT of chest, abdomen and pelvis showed no organomegaly, lymphadenopathy or hemorrhage. Right lower and upper extremity angiography revealed ulnar and popliteal artery thrombosis. The patient was transfused blood and treated with t-PA. Nevertheless he underwent amputation of his lower limb and right index and ring fingers. Dilemma remained as despite of adequate treatment patient leukocytosis, eosinophilia and lactic acidosis, persisted.
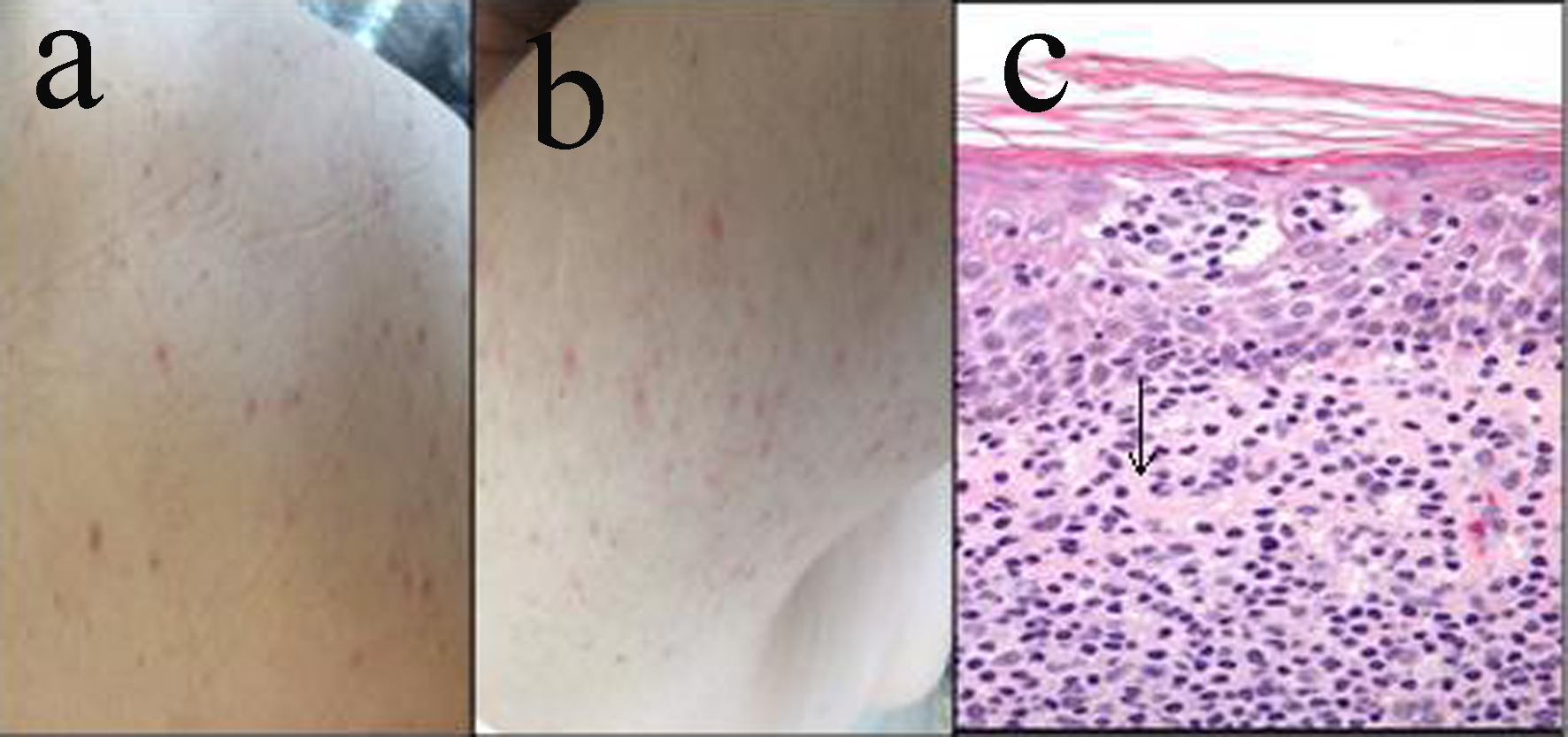 Click for large image | Figure 1. (a, b) Rash associated with Lennert lymphoma. (c) Histology of Lennert lymphoma, arrow showing epithelioid cell cluster. |
Since there was a high likelihood of hematological malignancy the patient underwent extensive workup. Bone marrow PCR gene rearrangement study revealed the presence of clonal population of T cells, consistent with T-cell leukemia. Immunophenotype staining showed CD 45+, 38+, 34+ and 117+. Skin biopsy revealed clusters of epithelioid cells intermingled with small lymphocytes (Fig. 1c). He was started on cyclophosphamide, doxirubucin, vincristine and prednisone. Chemotherapy resulted in resolution of rash and lactic acidosis and improvement of the hematological picture.
| Discussion | ▴Top |
Lennert lymphoma is a subtype of PTCL, NOS, which accounts for 6% of non-Hodgkin lymphomas. The immunophenotype of PTCL varies greatly and demonstrates expression of pan-T-antigens (CD2, CD3, CD5 or CD7). Roughly half cases present aberrantly with loss of pan-antigens [2], as in our patient. Clinical presentation includes lymphadenopathy, systemic B symptoms, eosinophilia or hemophagocytosis.
Eosinophilia occurs as a reaction to leukemia and has been reported as rare cause of arterial and venous thrombosis. The thrombotic event is induced by an eosinophile, which inhibits thrombomodulin function. Thrombomodulin serves as a cofactor for activation of protein C. Thus deficiency of activated protein C engenders a prothrombotic environment. This can explain the multi-organ thrombosis in our patient despite of having a therapeutic INR, as assessment of PT does not reflect levels of endogenous anticoagulants such as protein C [3].
Type B lactic acidosis is related to increased tumor burden and is associated with acute exacerbation of leukemias. Lactic acidosis originating from malignancies does not respond to usual resuscitative measures such as fluids and antibiotics and resolves only with chemotherapy.
Conclusion
The current poor prognostic factors for PTCL include age > 60, elevated serum lactate dehydrogenase, Eastern Cooperative Oncology Group (ECOG) Performance Status > 2 and bone marrow involvement [4]. Considering the wide spectrum of presenting symptoms, progressive nature and frequent relapses of the disease, it is thus imperative to have high index of clinical suspicion for “Lennert lymphoma” as early treatment has significant morbidity and mortality benefits. Also it may be a reasonable thought to widen the set of hematological prognostic factors for PTCL, NOS such as “lactic acidosis, eosinophila and leukocytosis” as in our patient.
Funding
None.
Conflict of Interest
None.
| References | ▴Top |
- Abouyabis AN, Shenoy PJ, Lechowicz MJ, Flowers CR. Incidence and outcomes of the peripheral T-cell lymphoma subtypes in the United States. Leuk Lymphoma. 2008;49(11):2099-2107.
doi pubmed - Weiss LM, Crabtree GS, Rouse RV, Warnke RA. Morphologic and immunologic characterization of 50 peripheral T-cell lymphomas. Am J Pathol. 1985;118(2):316-324.
pubmed - Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. 2011;365(2):147-156.
doi pubmed - Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, Morabito F, et al. Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood. 2004;103(7):2474-2479.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


