| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 3, Number 4, December 2014, pages 121-123
Occult B-Cell Lymphoma Associated With Hemophagocytic Syndrome: A Case Report
Jayashankar Erukkambattua, d, Shailaja Prabhalaa, Swamy Miryalab, Srinivas Maddalic, Ramamurti Tanikellaa
aDepartment of Pathology, Kamineni Academy of Medical Sciences and Research Centre, LB Nagar, Hyderabad 500068, India
bDepartment of General Medicine, Kamineni Academy of Medical Sciences and Research Centre, LB Nagar, Hyderabad 500068, India
cDepartment of Medical Oncology, Kamineni Academy of Medical Sciences and Research Centre, LB Nagar, Hyderabad 500068, India
dCorresponding Author: Jayashankar Erukkambattu, Quarter No. 7, Kamineni Doctors Quarters, Kamineni Hospitals, LB Nagar, Hyderabad 500068, India
Manuscript accepted for publication October 17, 2014
Short title: B-Cell Lymphoma
doi: http://dx.doi.org/10.14740/jh176w
| Abstract | ▴Top |
B-cell lymphomas associated with hemophagocytic syndrome (HPS) are quite rare. Here, we report a case of an occult B-cell lymphoma that was associated with HPS in a 56-year-old female. The presentation was of short duration and the clinical picture was dominated by features of overwhelming HPS leading to death of the patient.
Keywords: Hemophagocytic syndrome; Lymphoma; B cell
| Introduction | ▴Top |
B-cell lymphomas associated with hemophagocytic syndrome (HPS) are quite rare. HPS is a clinicopathologic entity characterized by fever, hepatosplenomegaly, pancytopenia, proliferation of histiocytes with evidence of erythrophagocytosis, markedly elevated serum triglycerides, ferritin, lactate dehydrogenase (LDH) and hypofibrinogenemia [1, 2]. Most of the cases reported are of T-cell lymphoma associated with histiocytosis. B-cell lymphoma association is quite rare, and hence, we report this case of an occult B-cell lymphoma which was associated with HPS.
| Case Report | ▴Top |
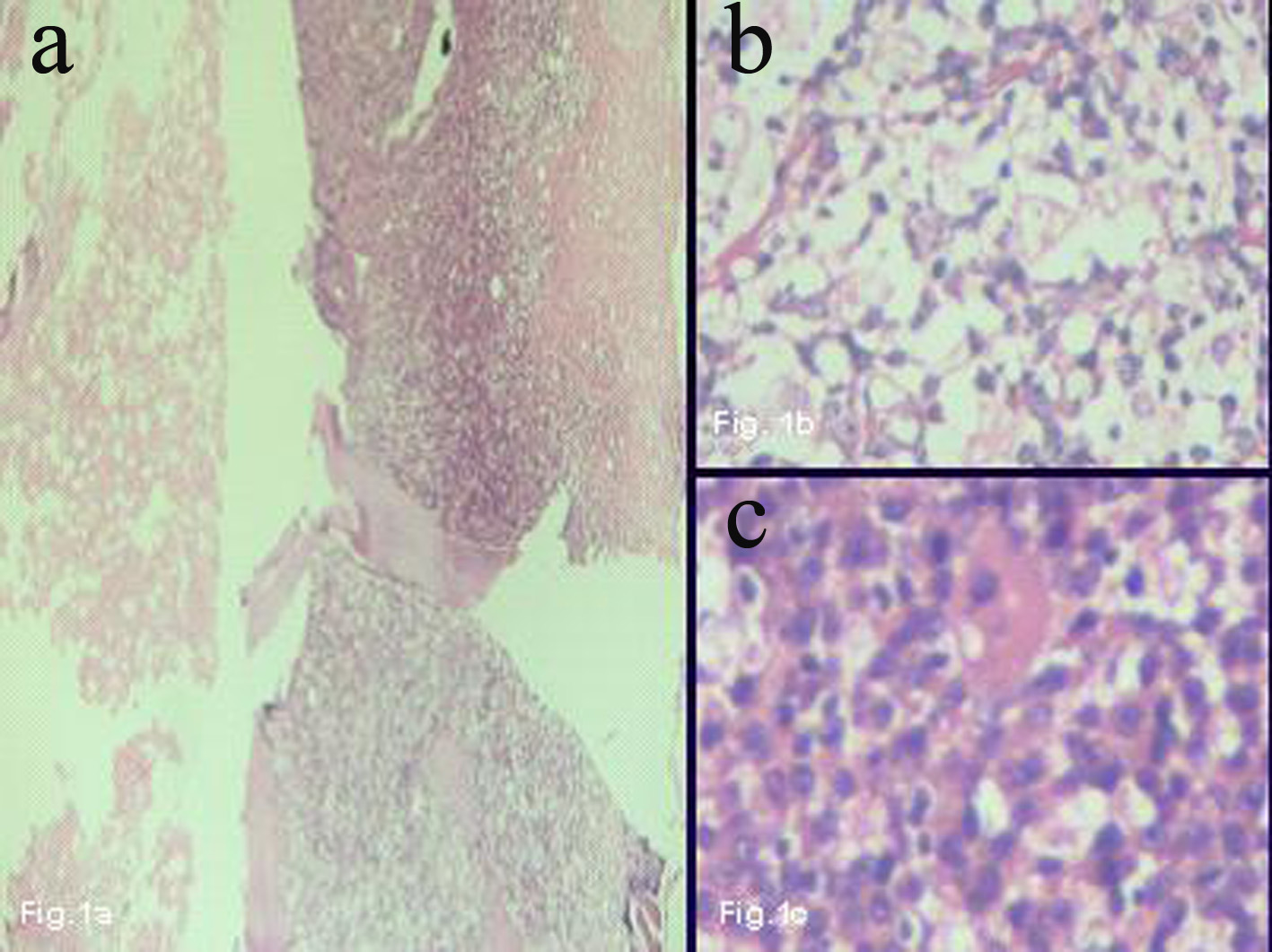
A 56-year-old female presented with history of recurrent fever, pain abdomen and pancytopenia over a period of 1 month. She had received six units of packed cell transfusion prior to admission. She was not a known case of diabetes mellitus, hypertension, asthma or epilepsy. On examination, she was moderately built, emaciated, pale and dehydrated. No icterus/cyanosis/generalized lymphadenopathy was noted. Pulse rate was 120/min, respiratory rate was 28/min, and temperature was 99 °F. Lungs showed bilateral crepitations and wheeze. Abdomen was distended moderately. Rest of the systems were within normal limits. Ultrasonogram/computerized tomography revealed mild bilateral pleural effusion and interstitial pneumonia. Her complete blood picture revealed 6.9 g/dL hemoglobin, 3,500/mm3 white cell count, and 60,000/mm3 platelets. Her erythrocyte sedimentation rate was raised (91 mm/hr), and urea (110 mg/dL), serum triglycerides (2,105 mg/dL), ferritin (9,543 ng/mL) and LDH (3,471 IU/mL) were markedly elevated. The serum was negative for antibodies, C-ANCA and P-ANCA. No organisms were grown in blood cultures. Bone marrow aspiration yielded a dry tap. Trephine biopsy was done which was adequate, and revealed large areas of necrosis, with a focus of viable area with prominence of histiocytes showing erythrophagocytosis and diffuse sheets of large plasmacytoid lymphocytes having round to oval nuclei with prominent nucleoli and moderate amount of amphophilic cytoplasm. The erythroid, myeloid and megakaryocytic series were markedly decreased (Fig. 1). Immunohistochemistry revealed CD20 positivity in large lymphoid cells, CD68 positivity in histiocytes (Fig. 2). Few cells (5-10%) showed CD5 positivity. Based on bone marrow biopsy, immunohistochemical findings and clinical presentation, a diagnosis of B-cell lymphoma associated with HPS was made. She was put on steroids and etoposide. In spite of treatment, her general condition gradually deteriorated, and she finally succumbed to respiratory failure within a short span of 3 days.
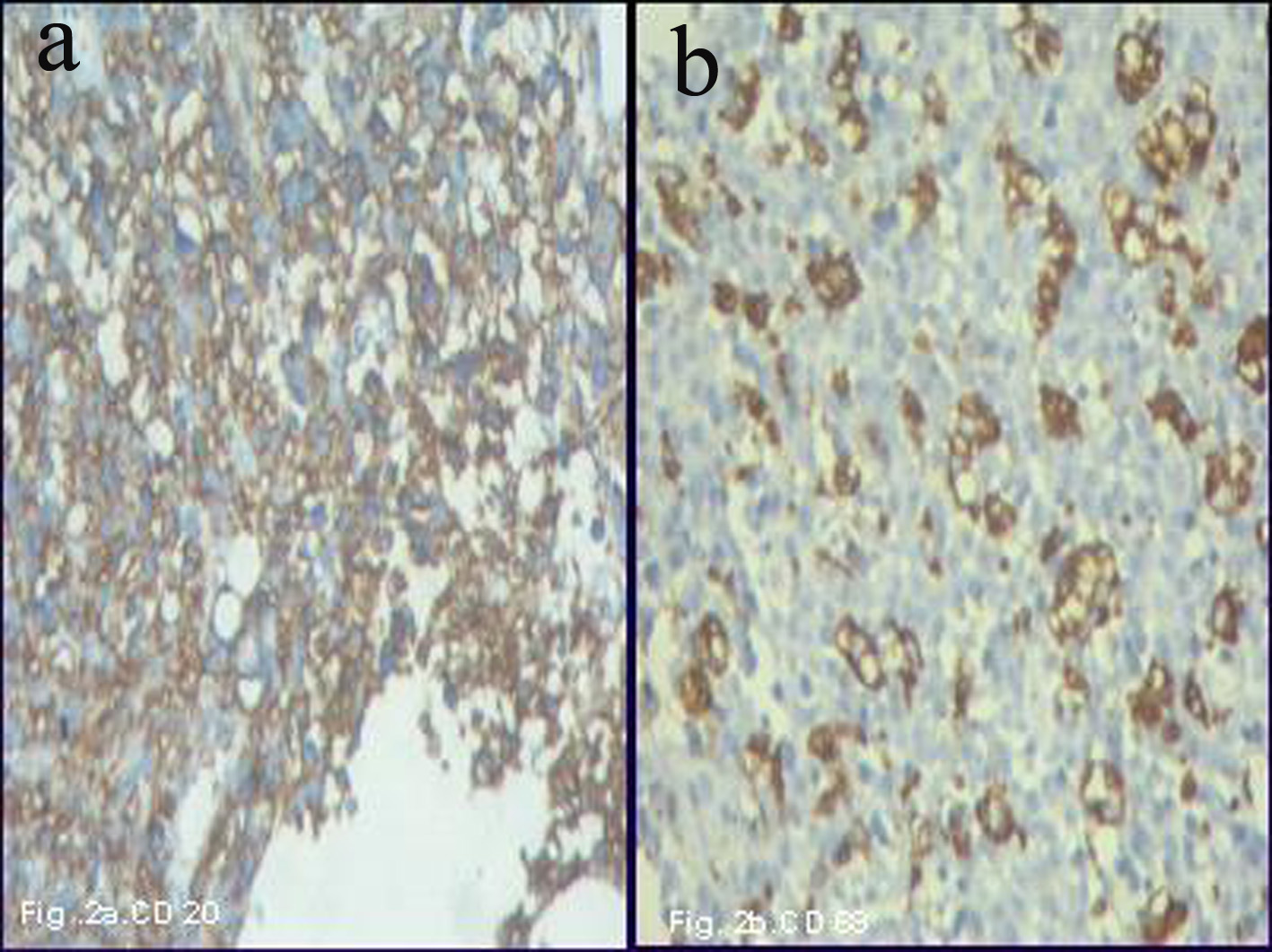 Figure 2. (a) Immunohistochemical test with CD20 shows diffuse positivity in the large lymphoid cells (× 400). (b) Immunohistochemical test with CD68 shows positivity in the histiocytes (× 400). Figure 2. (a) Immunohistochemical test with CD20 shows diffuse positivity in the large lymphoid cells (× 400). (b) Immunohistochemical test with CD68 shows positivity in the histiocytes (× 400). |
| Discussion | ▴Top |
Most cases of HPS caused by hematologic malignancies are associated with T-cell lymphomas while B-cell lymphoma association with HPS is quite rare [1, 2].
In our case, the occult B-cell lymphoma presented as HPS similar to the case reported by Kim et al [3]. In peripheral T-cell lymphoma, HPS occurrence is due to cytokines secreted by neoplastic T cells. However, in B-cell lymphomas no explanation is available. It can be attributed to the possibility of cytokine secretion from macrophages/B cells resulting in HPS [1, 3].
Viruses are common causes of HPS and the likely mechanism could be viral stimulated production of soluble macrophage/histiocyte activation factors with secondary histiocytic activation [3]. Altaf et al [4] reported a case of diffuse large B-cell lymphoma with Epstein-Barr virus-driven hemophagocytic lymphohistiocytosis. Miyahara et al [5] suggested a pathogenesis for HPS suggesting that hypercytokinemia is induced by proliferation of reactive CD8+ T cells.
HPS with lymphoma is characterized by high fever, cytopenia, elevated levels of LDH, ferritin, triglycerides, low fibrinogen levels and increased cytokines without evidence of infection [5, 6]. Our case presented with similar findings except that we did not perform estimation of cytokines.
HPS shows systemic activation of benign macrophages with extensive phagocytosis of hemopoietic cells [6], which explains pancytopenia and the need for multiple transfusions as seen in our case. Secondary HPS is more frequent than primary (familial), usually described in patients with an underlying disease [7]. In our case, no such condition was present. Hence we can attribute the occurrence of HPS to B-cell lymphoma, which was occult as well as extranodal, since there was no evidence of lymph nodal enlargement in the patient.
Diffuse large B-cell lymphoma complicated by HPS shows early relapse despite the treatment, indicating a need for more aggressive therapy [8]. In our case, the patient showed unfavorable outcome despite intense therapy.
Conclusion
Occult B-cell lymphoma can present with HPS. They do not respond well to treatment and carry a poor prognosis. One should have a high index of suspicion for occult hemopoietic malignancy when a patient presents with HPS.
Funding Support
Nil.
Conflict of Interest
Nil.
| References | ▴Top |
- Wilson MS, Weiss LM, Gatter KC, Mason DY, Dorfman RF, Warnke RA. Malignant histiocytosis. A reassessment of cases previously reported in 1975 based on paraffin section immunophenotyping studies. Cancer. 1990;66(3):530-536.
doi - Henter JI, Elinder G, Ost A. Diagnostic guidelines for hemophagocytic lymphohistiocytosis. The FHL Study Group of the Histiocyte Society. Semin Oncol. 1991;18(1):29-33.
pubmed - Kim JE, Kim CW, Park SH, Chi JG. Hemophagocytic syndrome associated with occult B-cell lymphoma: an autopsy case. J Korean Med Sci. 1998;13(1):77-80.
doi pubmed - Altaf S, Atreaga GM, Joshi AY, Rodriguez V. Diffuse large B-cell lymphoma in an adolescent female presenting with Epstein-Barr virus-driven hemophagocytic lymphohistiocytosis: a case report. J Med Case Rep. 2012;6:141.
doi pubmed - Miyahara M, Sano M, Shibata K, Matsuzaki M, Ibaraki K, Shimamoto Y, Tokunaga O. B-cell lymphoma-associated hemophagocytic syndrome: clinicopathological characteristics. Ann Hematol. 2000;79(7):378-388.
doi pubmed - Janka GE. Hemophagocytic syndromes. Blood Rev. 2007;21(5):245-253.
doi pubmed - Tzannou I, Balta AM, Bakiri M. Hemophagocytic syndrome associated with hematologic malignancies. Hospital Chronicles. 2011;6(3):110-117.
- Li X, He Y, Wang D, Hu Y, Wang W, Huang R. A case of diffuse large B-cell lymphoma complicated by hemophagocytic syndrome. Clin Lab. 2014;60(4):681-683.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.