| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Original Article
Volume 4, Number 3, September 2015, pages 187-192
Arterial and Venous Estimation of Hemoglobin: A Correlational Study
Farhan Al Enezia, Abdullah Al Anazia, Mohammed Al Mutairia, Mohammed Al Shahrania, Shoeb Qureshia, Manjush Karthikaa, b, c
aKing Saud bin Abdul-Aziz University for Health Sciences, King Abdul-Aziz Medical City, Riyadh, 11426, Kingdom of Saudi Arabia
bSymbiosis International University, Pune, India
cCorresponding Author: Manjush Karthika, King Saud bin Abdul-Aziz University for Health Sciences, King Abdul-Aziz Medical City, Ministry of National Guard Health Affairs, PO Box 22490, Riyadh, 11426, Kingdom of Saudi Arabia
Manuscript accepted for publication July 31, 2015
Short title: Arterial and Venous Estimation of Hemoglobin
doi: http://dx.doi.org/10.14740/jh224e
| Abstract | ▴Top |
Background: The objective of this study was to identify the correlation between arterial blood gas (ABG) hemoglobin and venous hemoglobin in acutely ill patients.
Methods: This was a prospective observational study on ABG and venous hemoglobin in samples drawn from 103 (59 males and 44 females) patients who presented to acute care areas like emergency room and intensive care units of a quaternary care center. ABG hemoglobin was estimated from point of care testing and venous hemoglobin was obtained from the sample sent to the laboratory. The data were entered into a specifically designed database and analyzed statistically by statistical package for the social sciences (SPSS) version 20.
Results: Although there were some serious pathological involvement and associated comorbidities, statistical analysis on correlation between ABG and venous hemoglobin showed a strong positive correlation between ABG and venous hemoglobin (P < 0.01).
Conclusion: ABG analysis of hemoglobin could be considered as an alternate tool for hemoglobin quantification, except in rarest scenarios that require a precise estimation of hemoglobin concentration. We also conclude that rapid estimation of hemoglobin by ABG analysis would enhance diagnostic approaches and prognostic aspects of critically ill patients.
Keywords: Hemoglobin; Arterial blood gas; Venous blood
| Introduction | ▴Top |
For the purpose of laboratory examinations, body fluids and secretions are collected from various sites of human body. Amongst these samples, blood is used routinely to detect for biochemical, hematological and immunological analysis. Certain blood parameters are measured by blood samples taken from either sites i.e. from vein and artery. Arterial and venous bloods are not quite similar. Blood count results are found to be different in arterial and venous sample, which included hematocrit and hemoglobin concentration, and the controversy remains the same about the exact aspects and mechanism of the difference [1].
Blood drawn from a skin puncture is a mixture of blood from veins, capillaries and arterioles; therefore it contains some amount of interstitial and intracellular fluid [2-4]. Though some studies have shown minimal differences in free flow of blood [1], others have shown definite differences in blood composition between skin puncture and venous blood samples in neonates [5], children and adults [6]. The differences may be exaggerated by cold atmosphere with resulting stasis of blood flow [2]. The routine and regular blood sampling in the critical care units may result in iatrogenic etiology of blood loss [7, 8]. This can worsen acute anemia, which is usually found in intensive care unit (ICU) patients with active hemorrhage, hemodilutional anemia or with bleeding diathesis [9]. Arterial blood gas (ABG) analyzers are one amongst the important diagnostic tools of all acute care settings, including ICU and emergency departments. Points of care (POC) ABG analyzers provide values of hemoglobin, glucose and electrolytes along with acid-base balance. ABG analysis has been found to be the most regularly and frequently ordered test in ICU [10] and has become an integral part in managing ICU patients. Critical care guidelines recommend 24 h of ABG availability [11].
Arterial and venous hemoglobin values are commonly used lab parameters in the clinical setup to monitor anemic insults and to guide decisions of transfusion. It was observed that awaiting venous hemoglobin may result in significant delay in diagnosis and management, thus dependence on ABG analysis of hemoglobin determination is increasing. As the consistency and accuracy of hemoglobin determination with ABG analyzers are less known, we prospectively analyzed its use in our hospital ICU settings, by choosing both ABG and venous blood samples to assess and compare any variation in the hemoglobin levels.
| Methodology | ▴Top |
Institutional review board of King Abdullah International Medical Research Center had given ethical clearance for this study. This observational cross-sectional study was conducted in the adult ICU and emergency department of King Abdulaziz Medical City (KAMC), Riyadh, Saudi Arabia. The ABG and venous blood samples were drawn from 103 time-matched patients who needed the estimation of hemoglobin. Arterial samples were obtained via arterial puncture or arterial line sampling in pre-heparinized blood gas syringes. The analysis of hemoglobin from ABG sample was done automatically with blood gas sampling in the ABG analyzer (COBAS B 221) of acute care settings, and the reports were printed immediately. The samples for venous hemoglobin analysis were transported through a rapid transit pneumatic system to the central laboratory for analysis. The analysis of hemoglobin from central laboratory was done by direct spectrophotometric measurement (SIEMENS ADVIA 2120). Those subjects who were healthy and normal as well as children less than 18 years were excluded from the study. All patients who required ABG sampling on the basis of their clinical presentation were included in the study. Patients with age 18 years or more were included from both genders (male 59, female 44) and most of the patients belonged to respiratory disorders, cardiovascular involvement, trauma, post-operative, septicemia, and potential metabolic problems such as diabetes and renal failure, and seizure disorders. Various parameters like demographic characteristics of the patients, diagnosis, time of obtaining the blood sample and the type of blood sample were noted. Data were presented in the form of mean, frequencies and percentages. The data were entered into a specifically designed database and analyzed statistically by statistical package for the social sciences (SPSS) version 20.
| Results | ▴Top |
A total of 103 patients admitted to the ICU and emergency department of KAMC due to various disease conditions were evaluated for the correlation between their ABG hemoglobin and venous hemoglobin. The frequencies of patients in the age groups 14 - 30 years, 31 - 50 years, 51 - 70 years and 71 - 90 years were 17, 16, 26 and 44 respectively (Fig. 1). The gender-wise distribution showed male (n = 59) to female (n = 44) ratio as 1.34 (Fig. 2). The distributions of diseases of the patients were 29 (respiratory disorders), 21 (cardiovascular complications), nine (trauma cases), eight each (CNS and gastrointestinal diseases), seven each (oncology and sepsis conditions), five (diabetes), three each (abdominal and renal disorders), two (hematological disorders) and one (amputation above right knee) (Table 1). There were no comorbidities found in 38 patients, while the highest comorbidities (39) were in diabetes plus hypertension group. The other comorbidities were hypertension alone (five), diabetes, hypertension and bronchial asthma (four), diabetes alone (three), bronchial asthma alone (three), diabetes, hypertension, coronary artery disease (two), diabetes, hypertension, congestive heart failure, and bronchial asthma (two), while the other comorbidities were one each (Table 2, Fig. 3). SPSS analysis on correlation between ABG and venous hemoglobin showed a strong positive correlation between ABG and venous hemoglobin (P < 0.01) (Table 3, Fig. 4).
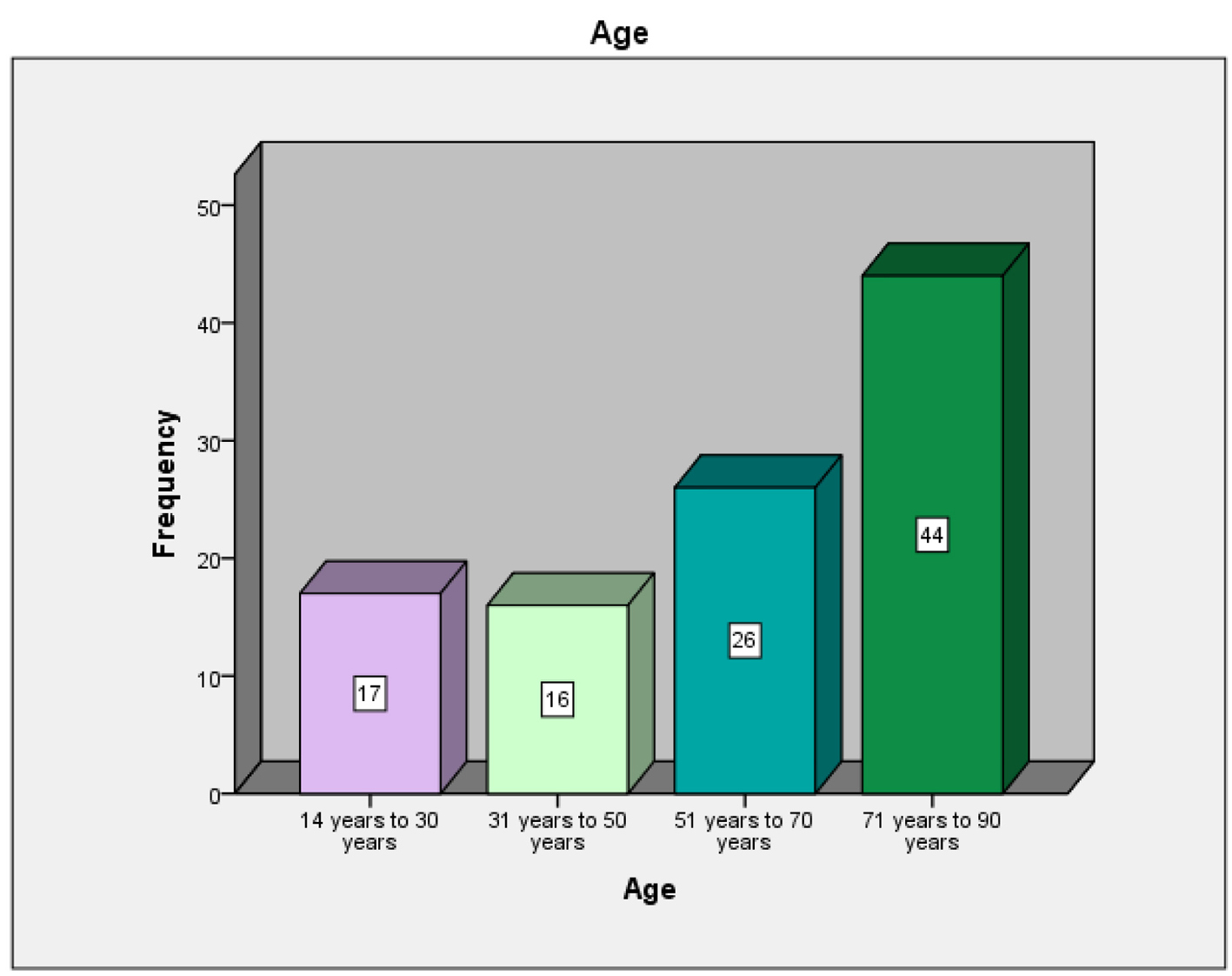 Click for large image | Figure 1. Frequency of different age groups of the patients whose ABG hemoglobin and venous hemoglobin were evaluated for correlation. |
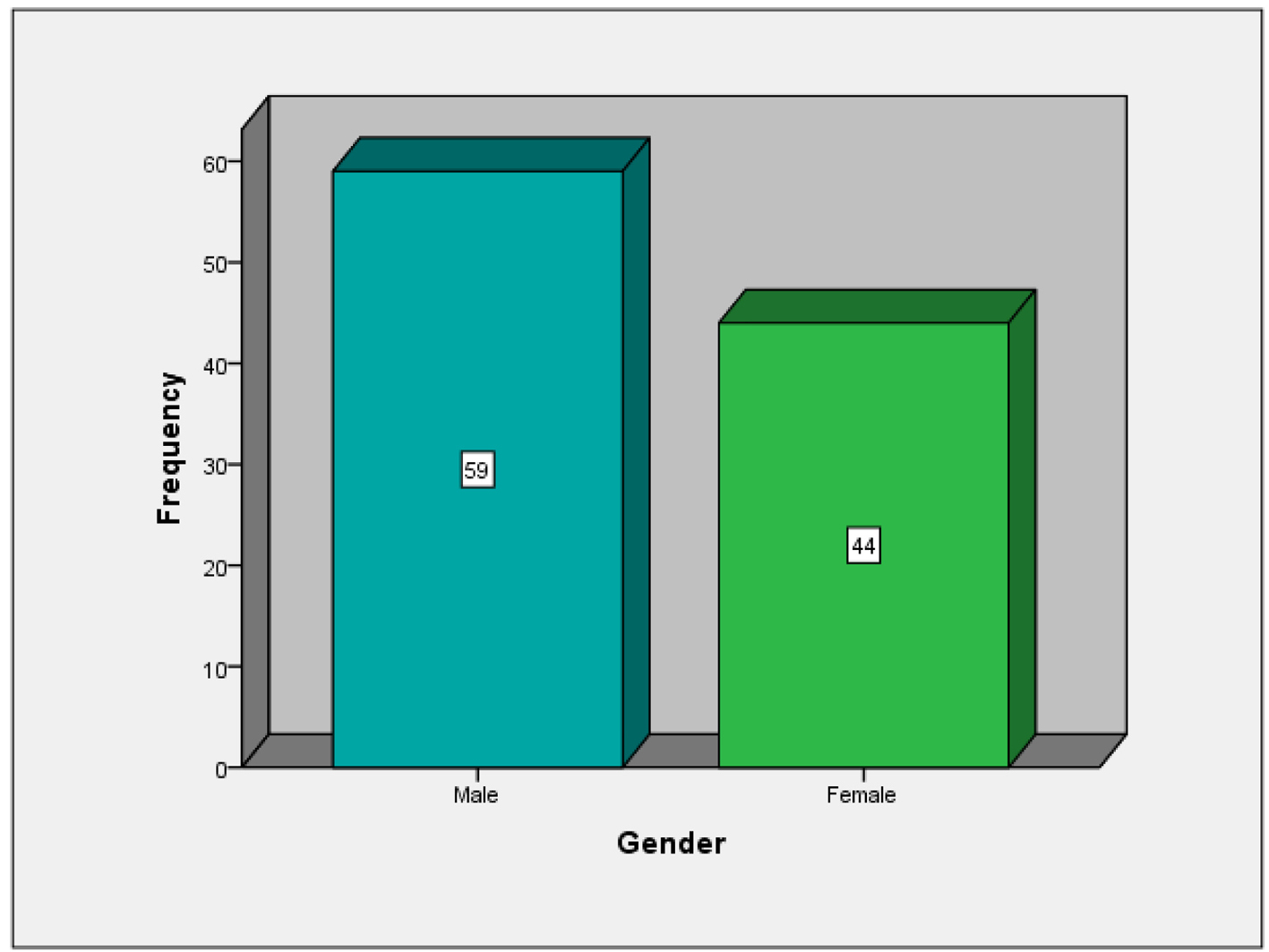 Click for large image | Figure 2. Gender distribution of the patients evaluated for correlation between ABG hemoglobin and venous hemoglobin. |
 Click to view | Table 1. Diagnosis of Different Diseases Among the Patients Whose ABG Hemoglobin and Venous Hemoglobin Were Evaluated for Correlation |
 Click to view | Table 2. Incidence of Comorbidities in the Patients Evaluated for Correlation Between ABG Hemoglobin and Venous Hemoglobin |
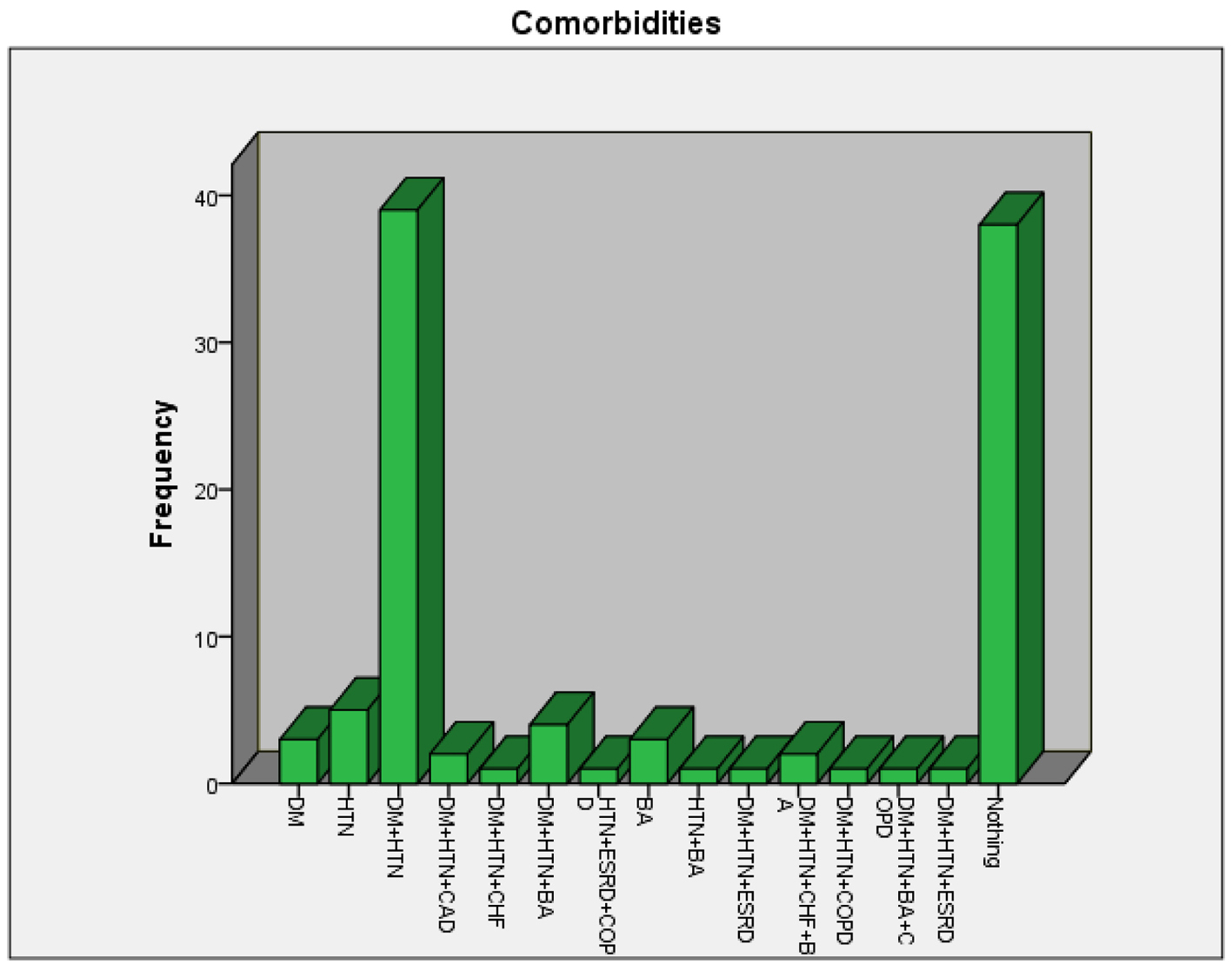 Click for large image | Figure 3. Incidence of comorbidities in the patients evaluated for correlation between ABG hemoglobin and venous hemoglobin. |
 Click to view | Table 3. Correlation Between ABG Hemoglobin and Venous Hemoglobin |
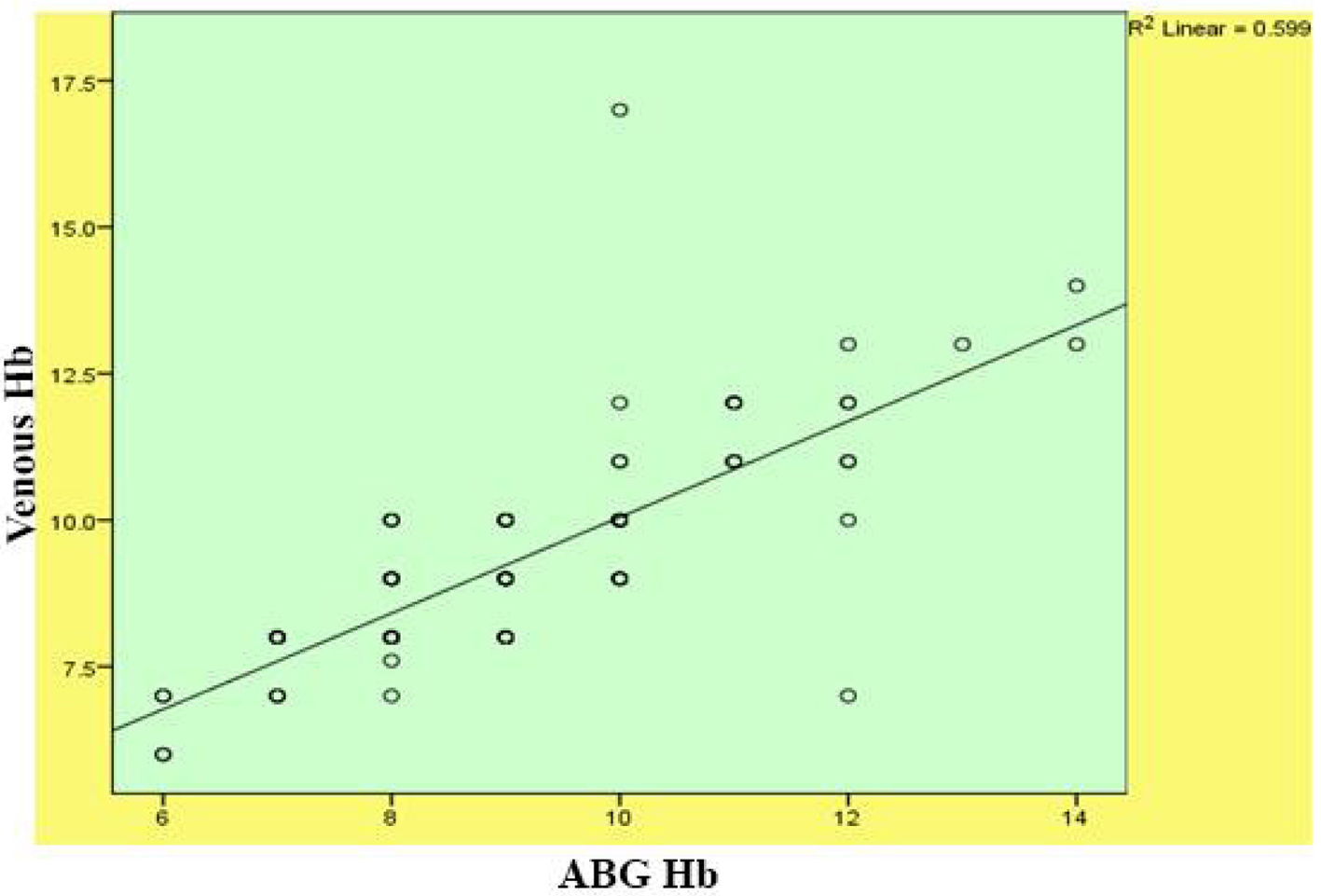 Click for large image | Figure 4. Scattered graph plotted to show the correlation between ABG hemoglobin and venous hemoglobin. |
| Discussion | ▴Top |
In the management of critically ill patients with hemodynamic and acid-base imbalance, ABG analysis has been considered as a keystone since its availability in early 1960s. ABG analysis provides instantaneous information about vital circulatory and respiratory physiologic variables and their derangements. World Health Organization defined anemia as hemoglobin level less than 13 g/dL in men and less than 12 g/dL in women [12]. It was observed that anemia affects one-quarter of the global population, nearly 50% of hospitalized patients, and up to 75% of hospitalized elderly patients [13]. A high percentage of patients become anemic during ICU stay, from 60% to 66% at admission [14, 15], up to 90% by day 3 [16] and 97% by day 8 [17]. The disturbances in the levels of hemoglobin can lead to serious toxic events, hence rapid and accurate assessment of these disturbances warrants fast medical attention. However, the quickness of the estimation and assessment of these parameters in the developing countries is frequently restricted by the irregularities in transport of samples to laboratories. Cox concluded that these impairements often negatively affect the samples and the related output [18].
In the present study, we aimed to evaluate the extent of correlation between ABG and venous blood sample for hemoglobin. If they are so, the data can be used alternately to perform the further practice. Notwithstanding of the differences that have been seen in how the ABG analyzer and venous sample machine work, our study showed that there is no significant differences in the analysis of ABG and venous hemoglobin levels. Various disease states included in the study were respiratory disorders, cardiovascular complications, trauma cases, post-operative cases, gastrointestinal diseases, diabetes, abdominal and renal disorders and hematological disorders. Some of the comorbid conditions were diabetes, hypertension, bronchial asthma and coronary artery diseases. Although there were some serious pathological involvement and associated comorbidities, there was a strong positive correlation between the ABG and venous hemoglobin. Our results are in agreement with the work of Ray et al who showed that an ABG analyzer may offer a substantial optional technique to the conventional Coulter counter for the assessment of hemoglobin levels in critically ill patients [19]. Our results are in contradiction with the conclusions of Yang et al who concluded that arterial hemoglobin levels were lower than venous samples, though it was not statistically significant [1]. The use of such alternative methods as a supplement to conventional laboratory testing will be a boon in getting quick and accurate results.
Conclusion
From our study, it is observed that the correlation between ABG and venous hemoglobin is found to be significant in blood samples taken from the patients suffering from different pathological conditions and associated comorbidities. Hence we would conclude that alternate methods of analyzing hemoglobin using ABG analyzers in the high dependent areas like ICUs and emergency departments will be an added advantage in providing early diagnosis and management including transfusions and achieving a better patient outcome. We also conclude that the use of such methods as a supplement to conventional laboratory testing will be a boon in getting fast and accurate results.
| References | ▴Top |
- Yang ZW, Yang SH, Chen L, Qu J, Zhu J, Tang Z. Comparison of blood counts in venous, fingertip and arterial blood and their measurement variation. Clin Lab Haematol. 2001;23(3):155-159.
doi pubmed - Van Assendelft OW, Simmons A. Specimen collection, handling, storage and variability, in Lewis SM, Koepke JA (eds): Hematology Laboratory Management and Practice. Oxford, Butterworth Heinemann, 1995, p 109-127.
- Conway AM, Hinchliffe RF, Earland J, Anderson LM. Measurement of haemoglobin using single drops of skin puncture blood: is precision acceptable? J Clin Pathol. 1998;51(3):248-250.
doi pubmed - Tatsumi N, Miwa S, Lewis SM. Specimen collection, storage, and transmission to the laboratory for hematological tests. Int J Hematol. 2002;75(3):261-268.
doi pubmed - Kayiran SM, Ozbek N, Turan M, Gurakan B. Significant differences between capillary and venous complete blood counts in the neonatal period. Clin Lab Haematol. 2003;25(1):9-16.
doi pubmed - Daae LN, Halvorsen S, Mathisen PM, Mironska K. A comparison between haematological parameters in 'capillary' and venous blood from healthy adults. Scand J Clin Lab Invest. 1988;48(7):723-726.
doi - Andrews T, Waterman H, Hillier V. Blood gas analysis: a study of blood loss in intensive care. J Adv Nurs. 1999;30(4):851-857.
doi pubmed - Drenck N. Point of care testing in Critical Care Medicine: the clinician's view. Clin Chim Acta. 2001;307(1-2):3-7.
doi - von Ahsen N, Muller C, Serke S, Frei U, Eckardt KU. Important role of nondiagnostic blood loss and blunted erythropoietic response in the anemia of medical intensive care patients. Crit Care Med. 1999;27(12):2630-2639.
doi pubmed - Muakkassa FF, Rutledge R, Fakhry SM, Meyer AA, Sheldon GF. ABGs and arterial lines: the relationship to unnecessarily drawn arterial blood gas samples. J Trauma. 1990;30(9):1087-1093; discussion 1093-1085.
- Guidelines for standards of care for patients with acute respiratory failure on mechanical ventilatory support. Task Force on Guidelines; Society of Critical Care Medicine. Crit Care Med. 1991;19(2):275-278.
doi pubmed - DeMaeyer E, Adiels-Tegman M. The prevalence of anaemia in the world. World Health Stat Q. 1985;38(3):302-316.
pubmed - Ania BJ, Suman VJ, Fairbanks VF, Rademacher DM, Melton LJ, 3rd. Incidence of anemia in older people: an epidemiologic study in a well defined population. J Am Geriatr Soc. 1997;45(7):825-831.
doi pubmed - Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, Meier-Hellmann A, et al. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288(12):1499-1507.
doi pubmed - Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Abraham E, MacIntyre NR, et al. The CRIT Study: Anemia and blood transfusion in the critically ill--current clinical practice in the United States. Crit Care Med. 2004;32(1):39-52.
doi pubmed - Gattinoni L, Chiumello D. Anemia in the intensive care unit: how big is the problem? Transfus Altern Transfus Med. 2002;4(4):118-120.
doi - Thomas J, Jensen L, Nahirniak S, Gibney RT. Anemia and blood transfusion practices in the critically ill: a prospective cohort review. Heart Lung. 2010;39(3):217-225.
doi pubmed - Cox CJ. Acute care testing. Blood gases and electrolytes at the point of care. Clin Lab Med. 2001;21(2):321-335.
pubmed - Ray JG, Post JR, Hamielec C. Use of a rapid arterial blood gas analyzer to estimate blood hemoglobin concentration among critically ill adults. Crit Care. 2002;6(1):72-75.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


