| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 5, Number 2, June 2016, pages 67-69
A 29-Year-Old Female With Hereditary Coproporphyria and New-Onset Seizures
Sabrina S. Sama, b, Karel T. S. Valentaa, Joshua J. Baiela
aMS3, Northwest Hospital, Randallstown, MD, USA
bCorresponding Author: Sabrina S. Sam, 6062 Green Meadow Parkway Apt A, Baltimore, MD 21209, USA
Manuscript accepted for publication March 14, 2016
Short title: HCP and New-Onset Seizures
doi: http://dx.doi.org/10.14740/jh258w
| Abstract | ▴Top |
Hereditary coproporphyria (HCP) by itself can pose significant diagnostic and management difficulties. Together with seizures and renal failure, management can be even more challenging. This poses a dilemma with treatment and requires a unique approach. Our patient is a 29-year-old Caucasian female with HCP who presented with new-onset seizures, diffuse abdominal pain and significant anion gap metabolic acidosis. She had a 7-year history of admissions for severe abdominal pain and was diagnosed with HCP 3 years ago. HCP is a rare disorder that can be complicated by seizures. Many anti-seizure medications can exacerbate acute porphyria attacks. To further complicate management, the anti-seizure drugs of choice in porphyrias are renally excreted and must be adjusted for renal function. Liver transplantation may be a last resort in patients with HCP and seizures.
Keywords: Hereditary coproporphyria; New-onset seizures; Renal failure
| Introduction | ▴Top |
Hereditary coproporphyria (HCP) is an autosomal dominant disorder of heme synthesis that is classified as a hepatic porphyria with both acute and chronic manifestations. It is an extremely rare condition, affecting more women than men, believed to be symptomatic in two per million people by one Danish study [1]. Although the disease is inherited in an autosomal dominant fashion, there is low penetrance. The lack of family history as well as the scarcity of HCP can lead to a delay in diagnosis. HCP can lead to neurologic manifestations during acute attacks as well as chronic cutaneous manifestations. Common precipitating causes of acute attacks include medication, specifically hepatic enzyme inducers, fasting, and increased progesterone [2].
HCP is caused by an enzymatic deficiency of coproporphyrinogen oxidase, an enzyme in the heme synthesis pathway. Acute attacks are thought to occur when this enzyme becomes the rate limiting step of the heme synthesis pathway [3]. Accumulation of its substrate, coproporphyrinogen, leads to both the acute attacks and photosensitivity seen in HCP. Coproporphyrinogen is an allosteric inhibitor of porphobilinogen deaminase. Inhibition of this enzyme results in increased precursors in the heme synthesis pathway including delta-amino levulinic acid (ALA) and porphobilinogen (PBG) (Fig. 1). Both ALA and PBG are neurotoxic substances that can cause neurologic symptoms present during acute attacks [4].
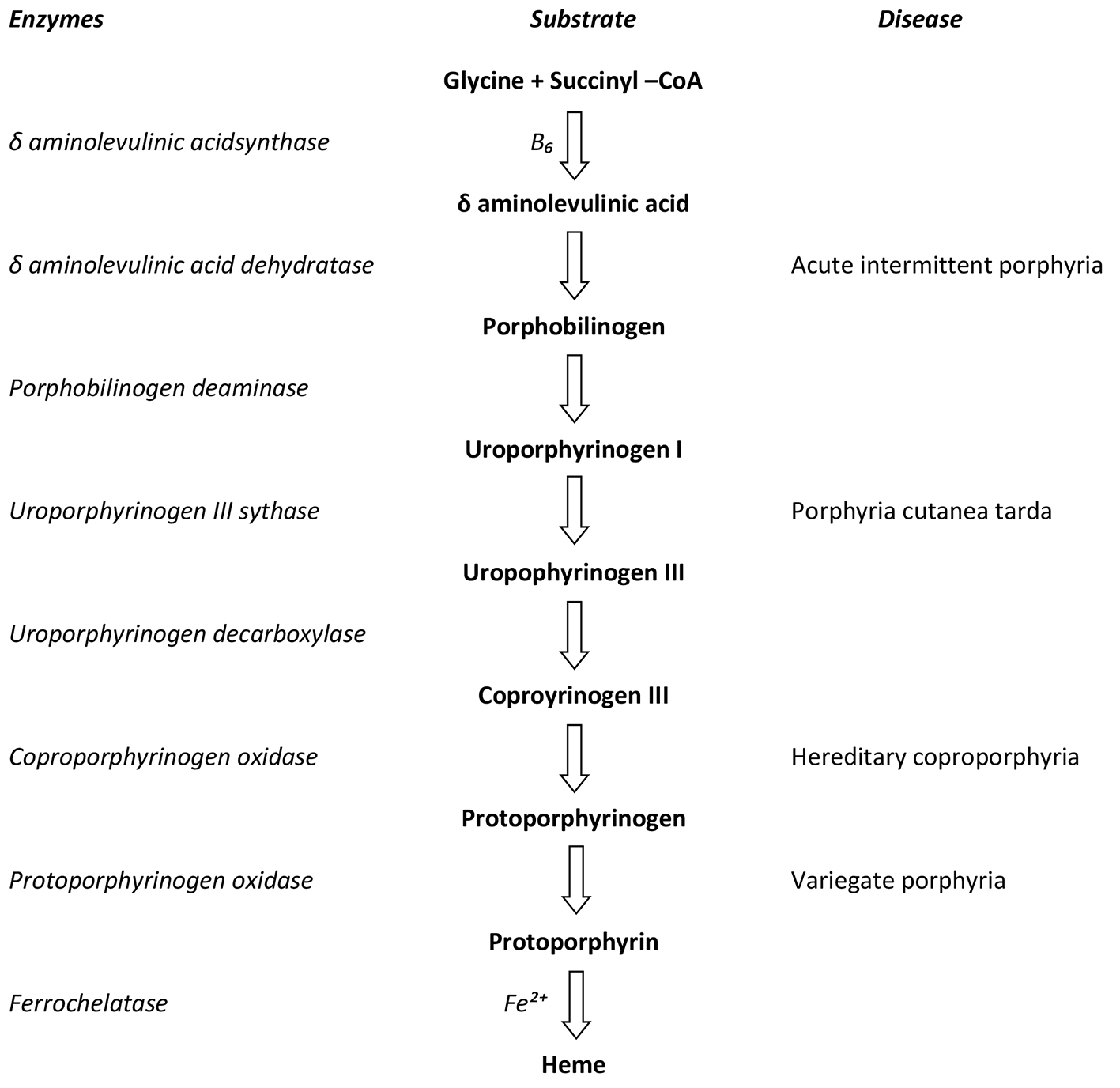 Click for large image | Figure 1. Pathway of heme synthesis including enzymes and associated porphyrias. Referenced from: Desnick RJ, Balwani M. The Porphyrias. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, Loscalzo J. Harrison’s Principles of Internal Medicine 19e. United States of America: McGraw-Hill Companies, Inc.; 2015. Figure 358-1. |
The most common symptom of acute HCP is severe abdominal pain with nausea and vomiting. Seizures, motor neuropathy, tachycardia, hypertension and constipation are also clinical symptoms seen in HCP [2, 5]. Photosensitivity is an uncommon presentation of HCP and resembles the signs of porphyria cutanea tarda and porphyria variegate. Additional late stage complications include renal disease and hepatocellular carcinoma [2].
| Case Report | ▴Top |
Our patient is a 29-year-old female with a past history significant for HCP and polycystic ovarian syndrome (PCOS) who presented to the emergency department (ED) with new-onset seizures and severe abdominal pain with nausea and vomiting. Two witnessed seizures occurred prior to arrival at the ED and were described as generalized tonic clonic seizures with tongue biting and incontinence. Another seizure ensued in triage and valproic acid was contemplated but not given. An additional seizure followed that night at which point neurology was consulted. They advised a loading dose of phenytoin followed by maintenance doses with further seizure activity. A CT scan and an MRI of the head did not reveal any abnormalities and an EEG was inconclusive for seizure activity.
In the ED, labs revealed an anion gap metabolic acidosis with a bicarbonate of 7 and a corrected anion gap of 21. Lactate, ethanol and blood sugar levels were all normal. The creatinine level was 7.23 and the metabolic acidosis was presumed to be due to acute on chronic renal failure, a possible complication of HCP [6].
Our patient had a long history of abdominal pain associated with acute attacks of HCP, occurring almost monthly for 7 years. These attacks were treated with hemin infusions and she did receive these upon admission. Subsequently, they were discontinued due to her renal dysfunction.
Additional findings included hypocalcemia, anemia, thrombocytopenia, leukocytosis and hypertension. Hypocalcemia and an elevated parathyroid hormone were thought to be secondary to renal failure. The etiologies of her hepatomegaly and anemia were most likely non-alcoholic fatty liver and splenomegaly, respectively. Thrombocytopenia was a chronic problem for our patient and was believed to be due to either splenomegaly or immune thrombocytopenic purpura. Our patient also had photosensitivity that led to blistering and peeling upon presentation that resolved during her hospital stay.
| Discussion | ▴Top |
There are many unsafe drugs in porphyrias (Table 1). According to Rare Clinical Disease Research Network, a few of the most harmful include OCPs, sulfonamide antibiotics, rifampin, barbiturates and anti-seizure medications. Seizures in patients with HCP can be dangerous if not treated appropriately. Valproate and phenytoin are both unsafe medications in HCP, and can lead to increased exacerbations. Phenytoin is a hepatic enzyme inducer and can increase the activity of ALA dehydratase increasing substrate accumulation [2].
 Click to view | Table 1. Porphyria Drug Lists |
Gabapentin and levetiracetam are the drugs of choice in HCP; however, they both undergo renal excretion and require renal dosing [7, 8]. The exact mechanism in which HCP leads to renal failure is unknown, but it is thought to be related to nephrotoxic effects of porphyrin precursors [6]. Lamotrigine is an alternative anti-seizure medication for our patient according to the safe list available from the European Porphyria Network.
Our patient faces significant hardships in her medical management due to her coexisting conditions and her worsening exacerbations. Therefore, it may be beneficial to consider liver transplantation as it has proven beneficial in similar porphyrias. Despite the lack of documented liver transplantations in patients with HCP, the results available for other hepatic porphyrias are promising. A French case study describing the successful reduction of porphyrins in both the urine and stool following liver transplantation in a patient with variegate porphyria (VP) concludes that transplantation may be the only definitive treatment in the case of severe hepatic damage [9]. Given the similarities between HCP and other porphyrias treated with liver transplantation, we would recommend that our patient be considered a candidate for liver transplantation.
Conclusion
Multiple drug interactions must be considered in patients with HCP as many medications are considered unsafe in patients with porphyrias. These unsafe drugs can lead to a decrease in heme synthesis and precipitate acute attacks (Table 1). New-onset seizures can therefore lead to dilemmas in treatment. Phenytoin and valproic acid are both unsafe in patients with HCP, therefore, gabapentin and levetiracetam are the drugs of choice in HCP but require renal dosing. For our patient, lamotrigine is an alternative option if she has future seizures as it does not require renal dosing.
HCP is a rare disease that is relatively unknown to most physicians. Patients with HCP face significant hardships complicated when new symptoms create more difficult medial management. Our patient experiences increasing frequency and severity of acute attacks despite available medical management. Standard medical treatments may be inadequate so we feel that liver transplantation is a valid alternative that should be considered.
Acknowledgments
We would like to thank Dr. Karen Scott for her critical review of the manuscript.
Competing Interest
The authors declare that they have no competing interests.
| References | ▴Top |
- With TK. Hereditary coproporphyria and variegate porphyria in Denmark. Dan Med Bull. 1983;30(2):106-112.
pubmed - Bissell DM, Wang B, Lai J. Hereditary Coproporphyria. 2012 Dec 13 [Updated 2015 Jul 1]. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. Gene Reviews [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2015. Available from: http://www.ncbi.nlm.nih.gov/books/NBK114807/.
- Elder GH, Evans JO, Thomas N. The primary enzyme defect in hereditary coproporphyria. Lancet. 1976;2(7997):1217-1219.
doi - Meissner P, Adams P, Kirsch R. Allosteric inhibition of human lymphoblast and purified porphobilinogen deaminase by protoporphyrinogen and coproporphyrinogen. A possible mechanism for the acute attack of variegate porphyria. J Clin Invest. 1993;91(4):1436-1444.
doi pubmed - Brodie MJ, Thompson GG, Moore MR, Beattie AD, Goldberg A. Hereditary coproporphyria. Demonstration of the abnormalities in haem biosynthesis in peripheral blood. Q J Med. 1977;46(182):229-241.
pubmed - Marsden JT, Chowdhury P, Wang J, Deacon A, Dutt N, Peters TJ, Macdougall IC. Acute intermittent porphyria and chronic renal failure. Clin Nephrol. 2008;69(5):339-346.
doi pubmed - Zadra M, Grandi R, Erli LC, Mirabile D, Brambilla A. Treatment of seizures in acute intermittent porphyria: safety and efficacy of gabapentin. Seizure. 1998;7(5):415-416.
doi - Sirsi D, Safdieh JE. The safety of levetiracetam. Expert Opin Drug Saf. 2007;6(3):241-250.
doi pubmed - Stojeba N, Meyer C, Jeanpierre C, Perrot F, Hirth C, Pottecher T, Deybach JC. Recovery from a variegate porphyria by a liver transplantation. Liver Transpl. 2004;10(7):935-938.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


