| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 5, Number 2, June 2016, pages 76-78
Diffuse Kidney and Retroperitoneal Infiltration by Plasmablastic Myeloma
Maxime Touzota, d, Othman Laghmaria, Nicolas Blinb, Anne Moreauc, Fadi Fakhouria
aService de Nephrologie et Immunologie Clinique, ITUN, CHU Nantes, France
bService d’Hematologie, CHU Nantes, France
cService d’Anatomie et Pathologie, CHU Nantes, France
dCorresponding Author: Maxime Touzot, ITUN, 30 Boulevard Jean Monnet, 44000 Nantes, France
Manuscript accepted for publication May 23, 2016
Short title: Plasmablastic Myeloma
doi: http://dx.doi.org/10.14740/jh274w
| Abstract | ▴Top |
Plasmablatic cell myeloma is a rare but aggressive form of multiple myeloma (MM) with a poor survival. Extramedullary localization of plasmablastic myeloma may be observed in more than two-thirds of patients mainly in the upper digestive tract. Herein, we report the first case of plasmablastic MM leading to acute kidney injury through renal and ureteral infiltration.
Keywords: Myeloma; Acute kidny disease; Retroperitoneal infiltration
| Introduction | ▴Top |
Multiple myeloma (MM) is a malignant plasma cell neoplasm accounting for 10% of all hematologic cancers [1]. Extramedullary manifestations such as acute kidney injury (AKI) may reveal MM in 20% of patients. MM-associated AKI is usually secondary to intrarenal lesions such as cast nephropathy, amyloidosis, hypercalcemia, hypovolemia or drug toxicity [2]. Herein, we report on an unusual case of AKI due to ureteral obstruction by an extramedullary localization of a plasmablastic myeloma, an atypical and aggressive form of MM.
| Case Report | ▴Top |
A 67-year-old male patient was referred to our department for AKI in the setting of an MM relapse. Four years earlier, the patient received a course of proteasome inhibitor (bortezomib) and dexamethasone for an IgA MM, and underwent a successful autologous hematopoietic stem cell transplantation. He had been considered in complete hematological remission under lenalidomide as maintenance therapy.
On admission, the patient complained of abdominal pain, fluid overload, hypertension and oliguria. Serum creatinine was 635 µmol/L and 24-h proteinuira was 3.92 g. Other laboratory tests showed calcemia 2.4 mmol/L, bicarbonates 22 mmol/L, albumin 23 g/dL and C-reactive protein 20 mg/L, a generative normocytic anemia (hemoglobin 9.2 g/dL), leukopenia (total white blood cells at 3,450/mm3), but normal platelets count (277,000/mm3). Immunofixation revealed a monoclonal IgA kappa with an excess of free light chains (kappa chain 772 mg/L, lambda chain 50 mg/L) and Bence-Jones proteinuria was detected. The lactate dehydrogenase (LDH) level was 7.79 µkat/L (normal range, 2.25 - 3.75 µkat/L). Bone marrow aspiration was not performed as all clinical and biological findings were consistent with the diagnosis of MM relapse. Abdominal ultrasound showed enlarged kidneys without urinary tract obstruction.
The patient was started immediately on chemotherapy (dexamethasone and bortezomib). One week after initiation of therapy, he complained of dysuria. A bacterial prostatitis (Escherichia coli) was diagnosed and treated with parenteral antibiotics (piperacillin and tazobactam). He rapidely developed anuria requiring hemodialysis 7 days later. Despite hemodialysis, clinical symptoms worsened as he complained of abdominal pain associated with dyspnea. Abdominal CT scan identified a large retroperitoneal mass infiltrating both kidneys, compressing the ureters, and diffusing into the bladder (Fig. 1). The patient died 3 days later in the setting of uncontrolled sepsis.
 Click for large image | Figure 1. Abdominal CT scan. Large intra-abdominal mass arising from soft tissues and extending in the pelvic region. Dilatation of both ureters was noted. |
A biopsy of the retroperitoneal mass and kidney disclosed a diffuse infiltration of conjunctive tissues and kidney by CD138+ CD20- plasmacytoid cells with a high Ki67 expression (Fig. 2). The diagnosis of plasmablastic myeloma was made.
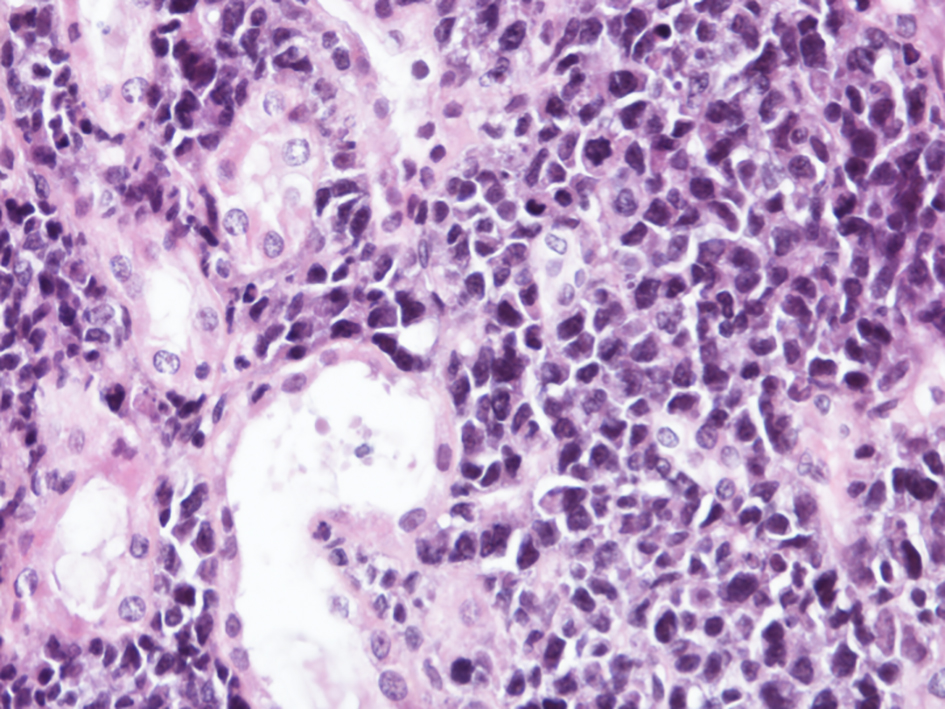 Click for large image | Figure 2. Kidney biopsy, light microscopy (HES, × 400). Diffuse an intense infiltration of the interstitium by plasmablasts. |
| Discussion | ▴Top |
MM is characterized by the clonal proliferation of plasma cells in the bone marrow and usually by the presence of a monoclonal Ig in the blood and/or the urine [1, 2]. In some patients, MM may take the form of plasmablastic myeloma, in which myeloma cells are detected in the circulation [3]. This plasmablastic transformation usually represents the terminal evolution of MM with a poor response to chemotherapy [3-6]. Plasmablastic myeloma cells are defined as having a fine reticular nuclear chromatin pattern, a large centrally placed nucleus (> 10 μm), a large nucleolus (> 2 μm) and a high nuclear/cytoplasmic ratio. The cytoplasm lacks a prominent perinuclear hof (area containing the Golgi apparatus) [6, 7].
Extramedullary localization of plasmablastic myeloma may be observed in more than two-thirds of patients [6] mainly in lymph nodes, the upper digestive tract, a common site of primary extramedullary plasmacytoma, and the central nervous system [6, 8]. Kidney involvement has been rarely reported [9].
Rare cases of AKI due to MM cells infiltrating the kidneys have been reported so far, within possible coexistent cast nephropathy [10-12]. To the best of our knowledge, this is the first case of plasmablastic MM leading to AKI through renal and peri-renal infiltration.
The rapid onset of ureteral obstruction, and the high proliferation of tumoral cells assessed by the Ki67 expression, reflect the aggressiveness of the plasmablastic form of MM.
Conclusion
Plasmablatic cell myeloma is a rare but aggressive form of MM with a poor survival. Plasmablastic tranformation should be considered in MM presenting with AKI, high level of LDH and kidney enlargement and/or obstruction.
Conflicts of Interest
None.
| References | ▴Top |
- Kyle RA, Rajkumar SV. Multiple myeloma. Blood. 2008;111(6):2962-2972.
doi pubmed - Singhal S, Mehta J. Multiple myeloma. Clin J Am Soc Nephrol. 2006;1(6):1322-1330.
doi pubmed - Carter A, Hocherman I, Linn S, Cohen Y, Tatarsky I. Prognostic significance of plasma cell morphology in multiple myeloma. Cancer. 1987;60(5):1060-1065.
doi - Piccinini L, Artusi T, Bonacorsi G, Arigliano V. Acute leukemia of plasmablastic type as terminal phase of multiple myeloma. Haematologica. 2002;87(2):EIM04.
pubmed - Fernandez de Larrea C, Kyle RA, Durie BG, Ludwig H, Usmani S, Vesole DH, Hajek R, et al. Plasma cell leukemia: consensus statement on diagnostic requirements, response criteria and treatment recommendations by the International Myeloma Working Group. Leukemia. 2013;27(4):780-791.
doi pubmed - Lorsbach RB, Hsi ED, Dogan A, Fend F. Plasma cell myeloma and related neoplasms. Am J Clin Pathol. 2011;136(2):168-182.
doi pubmed - Lee CK, Ma ES, Shek TW, Lam CC, Au WY, Wan TS, Chan LC. Plasmablastic transformation of multiple myeloma. Hum Pathol. 2003;34(7):710-714.
doi - Yadav S, Kumar R, Jaiyesimi IA, Chisti MM. Aggressive plasmablastic multiple myeloma in a 42-year-old: is inflammatory bowel disease or infliximab treatment to be blamed? BMJ Case Rep. 2013;2013.
- Srija M, Zachariah PP, Unni VN, Mathew A, Rajesh R, Kurian G, Neeraj S, et al. Plasmablastic myeloma presenting as rapidly progressive renal failure in a young adult. Indian J Nephrol. 2014;24(1):41-44.
doi pubmed - Hanawa S, Akimoto T, Uehara E, Inoue M, Imai T, Kotoda A, Yoshizawa H, et al. Renal failure caused by plasma cell infiltration in multiple myeloma. Clin Exp Nephrol. 2011;15(4):586-590.
doi pubmed - Adamidis KN, Charitaki EE, Christodoulidou C, Tasidou A, Hadjiconstantinou V. Nonsecretory multiple myeloma - a rare case of acute renal failure. Clin Nephrol. 2010;74(4):311-314.
pubmed - Nasr SH, Alobeid BB, Otrakji JA, Markowitz GS. Myeloma cast nephropathy, direct renal infiltration by myeloma, and renal extramedullary hematopoiesis. Kidney Int. 2008;73(4):517-518.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


