| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 7, Number 3, September 2018, pages 112-115
May-Thurner Syndrome: A Rare and Under-Appreciated Cause of Venous Thrombosis in a 18-Year-Old Healthy Female
Ryan L. Goetza, James Jae-Hyung Yoob, Joyce Hsua, Anusha Vakitic, David M. Hardyd, Khurram Tariqe, f
aMedical College of Georgia at Augusta University, 1120 15th Street, Augusta, GA 30912, USA
bDepartment of Medicine at Augusta University, 1120 15th Street, Augusta, GA 30912, USA
cDepartment of Internal Medicine, Medstar Washington Hospital Center, 110 Irving St NW, Washington, DC 20010, USA
dDepartment of Vascular Surgery at Augusta University, 1120 15th Street, Augusta, GA 30912, USA
eGeorgia Cancer Center, Augusta University, 1120 15th Street, Augusta, GA 30912, USA
fCorresponding Author: Khurram Tariq, Georgia Cancer Center, Augusta University, 1120 15th Street, Augusta, GA 30912, USA
Manuscript submitted February 5, 2018, accepted February 23, 2018
Short title: Recurrent Thrombosis in May-Thurner Syndrome
doi: https://doi.org/10.14740/jh381w
| Abstract | ▴Top |
May-Thurner syndrome (MTS) is a rarely diagnosed vascular abnormality that typically presents in young adults. The anomaly arises from compression of the left common iliac vein between the right iliac artery anteriorly and the lumbar vertebral body posteriorly, resulting in lower extremity venous outflow obstruction and recurrent deep vein thromboses (DVTs). We report the case of a 24-year-old female with a long history of recurrent DVTs and pulmonary emboli (PE) despite full anticoagulation. A computed tomography (CT) scan revealed findings consistent with MTS, and a left common iliac vein stent was placed. However, the patient continued to have DVTs while trialing several anticoagulation therapies, including rivaroxaban, enoxaparin, and warfarin. Eventually, the patient developed arterial thrombi resulting in critical limb ischemia, necessitating a right below knee amputation (BKA). One month status-post BKA, the patient was admitted for severe BKA stump pain secondary to infection and necrosis. She underwent BKA revision, but continued to experience pain post-operatively and was found to have new right common iliac artery, external iliac artery, and common femoral artery thrombosis in the setting of continued inpatient anticoagulation therapy with enoxaparin and aspirin. The patient returned to the operating room for emergent Fogarty thrombectomy, however, this was complicated by rupture of the balloon catheter secondary to migration of the left common iliac vein stent into the right common iliac artery lumen. A stent was placed in the right common iliac artery to shift the rogue vein stent, but the patient continued to have poor distal circulation of the BKA stump and eventually underwent an above knee amputation. Dual anti-platelet therapy (DAPT) with aspirin and clopidogrel in combination with enoxaparin were used to prevent in-stent thrombosis and future formation of arterial and venous thrombi. After the initiation of DAPT and enoxaparin, her clinical course was free of any further thromboembolic events. Clinicians should consider MTS in the differential diagnosis of younger adults presenting with recurrent DVTs or other unprovoked thromboembolic events. A two-pronged strategy of DAPT and anticoagulation was employed for successful prevention of thrombotic events.
Keywords: May-Thurner syndrome; Thrombosis; Dual anti-platelet therapy
| Introduction | ▴Top |
May-Thurner syndrome (MTS) is a rarely diagnosed vascular abnormality that typically presents in young adults. The anomaly arises from compression of the left common iliac vein between the right iliac artery anteriorly and the lumbar vertebral body posteriorly, thereby resulting in lower extremity venous outflow obstruction. May and Thurner first described this anatomic variant in 1957 as a “venous spur” and observed the aforementioned anomaly in 22% of cadavers [1]. Later, Cockett and Thomas further corroborated these findings in a study examining patients with acute left iliofemoral deep venous thrombosis (DVT) and subsequently renamed the condition “iliac vein compression syndrome” (IVCS) [2]. Although the prevalence of MTS is not well characterized, it is hypothesized that MTS-related DVTs account for 2% - 3% of all lower extremity DVT [3]. Additionally, MTS tends to develop in younger women, with current epidemiological studies showing that 72% of MTS cases are diagnosed between 25 to 50 years of age [3, 4].
| Case Report | ▴Top |
We report the case of a 24-year-old Caucasian female who first presented when she was 18 years old for the management of lower extremity pain and swelling. Over the years she developed multiple new DVTs and pulmonary emboli (PE), despite being fully anticoagulated. Computed tomography (CT) scan with angiography of her pelvis revealed a vascular abnormality consistent with MTS (Fig. 1). For the next 6 years, the patient experienced recurrent episodes of left lower extremity DVTs and PE requiring trials of various anticoagulation therapies, including rivaroxaban, warfarin, and enoxaparin. Additionally, multiple left common iliac vein stents and a supra-hepatic inferior vena cava filter were placed at an outside institution for the patient’s recurrent thromboembolic events. Eventually, the patient developed devastating complications including multiple episodes of critical limb ischemia of the right lower extremity which necessitated a below-the-knee amputation (BKA) at our institution 1 month prior to this hospital admission.
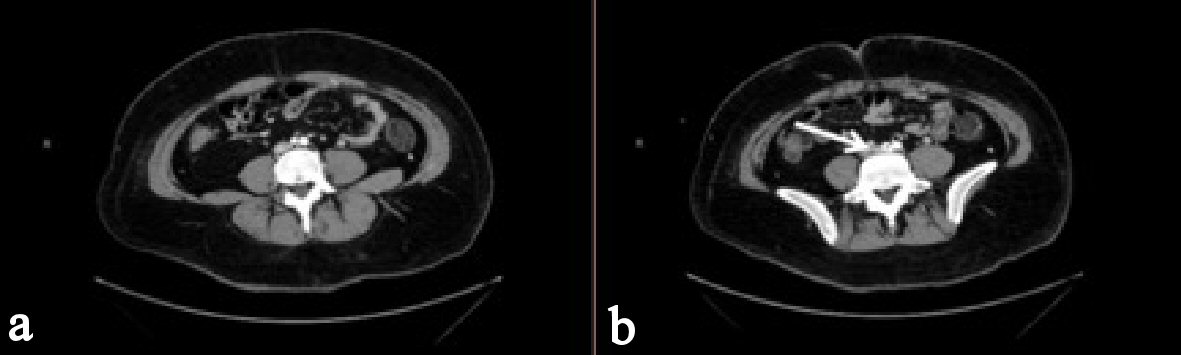 Click for large image | Figure 1. Axial CTA scans with intravenous contrast of the abdomen/pelvis. (a) Right common iliac artery crossing in front of left common iliac vein. (b) Compression of left iliac vein by the right iliac artery (white arrow). |
At age 24, the patient presented to the emergency department with complaints of severe pain at the site of her right BKA. At the time of presentation, she was being treated with enoxaparin for long-term anticoagulation. Physical examination was significant for tachycardia at 110 beats/min. The BKA site was without erythema or drainage, however, pain was elicited on palpation. The patient was otherwise afebrile and normotensive. She had an elevated white blood cell count of 19,000 cells/mm3. The results of other blood tests were within normal limits and PTT was appropriately elevated.
The patient was admitted and taken to the operating room for debridement of necrotic tissue and revision of BKA. Post-operatively, the patient was found to have new right-sided subtotal common iliac artery, external iliac artery, and common femoral artery thrombosis in the setting of continued inpatient anticoagulation therapy with enoxaparin and aspirin. Later during the hospital stay, the patient underwent Fogarty thrombectomy under fluoroscopy for these occlusions. The thrombectomy was complicated by migration of the previously placed left common iliac vein stent into the lumen of the right common iliac artery (Fig. 2). This resulted in repeated rupture of the balloon catheter as it was inflated and passed through this area of venous stent protrusion. Brisk arterial flow was eventually achieved by avoiding balloon inflation near the stent under fluoroscopic guidance. The arteriotomy was closed with a pericardial patch. An endovascular stent was then deployed in the right common iliac artery, which pushed the rogue left common iliac vein stent out of the lumen of the right common iliac artery. Subsequent angiography confirmed patency.
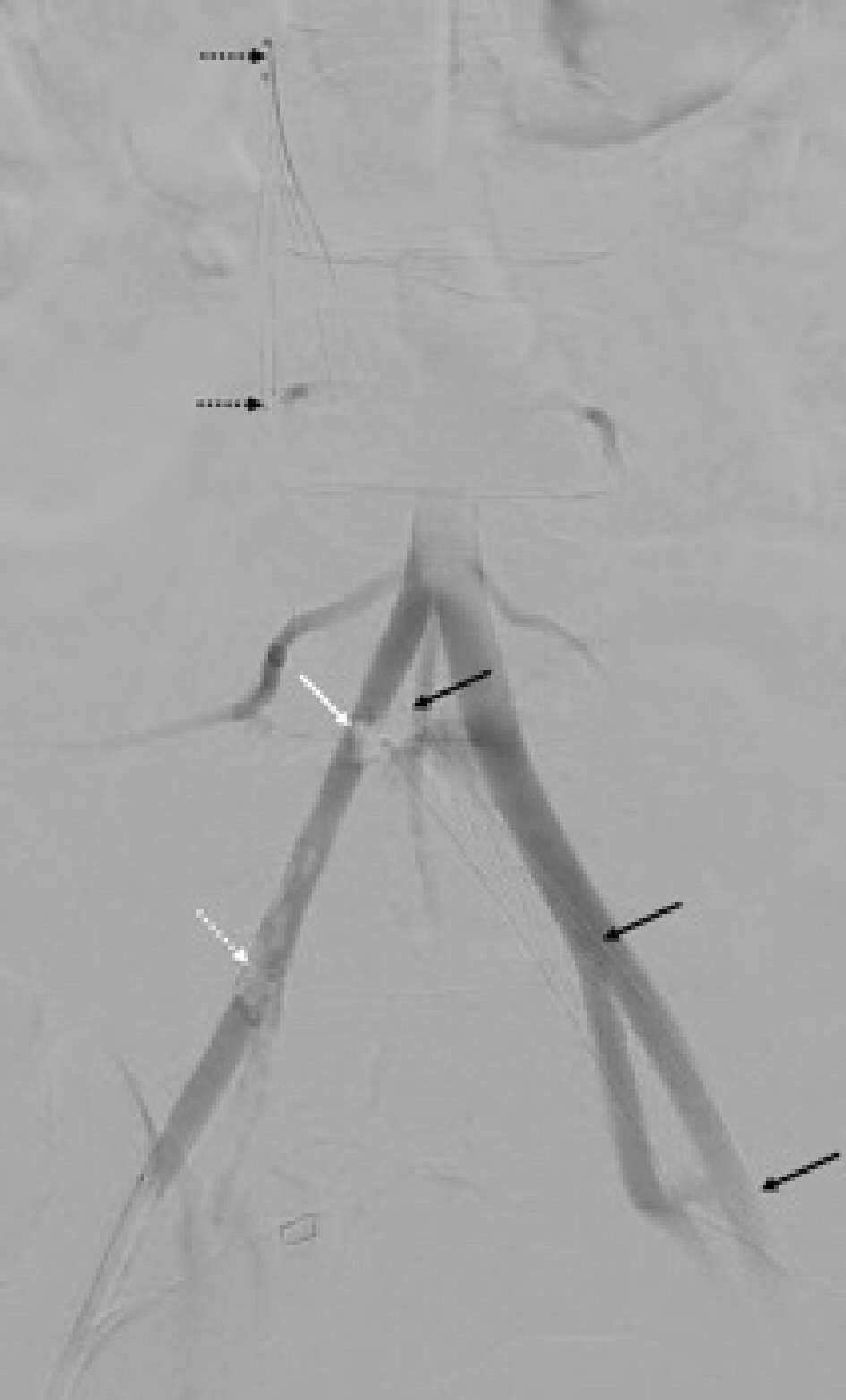 Click for large image | Figure 2. Intra-operative angiography demonstrating migration of the left common iliac vein stent (black arrows) into the lumen of the right common iliac artery with associated filling defect (white arrow). Filling defects consistent with arterial thrombi are also present distally (white dotted arrow). The inferior vena cava filter is seen in this image as well (dotted black arrows). |
Given her history of resistant hypercoagulable state, the Hematology and medical Oncology service was consulted for recommendations on long-term anticoagulation. Given the patient’s history of recurrent thromboembolic events in the setting of appropriate anticoagulation therapy with multiple agents, the decision was made to initiate dual-antiplatelet therapy (DAPT) with aspirin and clopidogrel in addition to anticoagulation with enoxaparin to prevent in stent-thrombosis and future formation and propagation of arterial and venous thrombi. At discharge, the patient was continued on DAPT along with enoxaparin. Patient’s post-hospitalization follow-up visits revealed no further development of DVTs or PEs. The patient returned to the emergency department 3 weeks after discharge with an infected, non-healing BKA. She was admitted for BKA debridement; however, the decision was ultimately made to perform a right above-the-knee amputation (AKA) for continued infection. The patient tolerated the AKA well and the stump proceeded to heal well.
| Discussion | ▴Top |
While MTS may manifest as an uncommon etiology of recurrent DVTs and PEs in the young adult population, the estimated prevalence rate of MTS found at autopsy may be as high as 22% to 32% [1, 2, 5]. Further literature review reveals a correlation between thrombophilia and MTS/IVCS. Kiernan et al found that among 30 IVCS patients, 12 patients had a positive thrombophilia workup including prothrombin gene mutation, factor V Leiden, anticardiolipin antibodies, antiphospholipid syndrome, and protein C and S deficiency [6]. In addition, Verhaeghe and Kolbel et al both have suggested association between MTS and genetic evidence of thrombophilia [7, 8]. Our patient had a pre-existing diagnosis of heterozygous factor V Leiden and lupus anti-phospholipid prior to her diagnosis with MTS. This may necessitate further epidemiological studies and exploration into various modes of surveillance of MTS in patients with evidence of thrombophilia.
The initial management of patients with symptomatic MTS or MTS-related DVTs with endovascular procedures remains the mainstay of treatment. Several case reports have explored surgical approaches to MTS. One study compared the efficacy of catheter-directed thrombolysis (CDT) versus percutaneous mechanical thrombectomy (PMT) in addition to percutaneous stenting [9, 10]. However, endovascular management alone is often insufficient for treatment of symptomatic MTS. A dual-therapeutic approach with endovascular intervention and pharmacotherapy with anticoagulation has steadily emerged as the new standard of care, often requiring a multi-disciplinary effort [11]. This has become especially relevant in light of post-vascular complications, including in-stent re-thrombosis. Birn and Vedantham characterized a post-surgical phenomenon called post-thrombotic syndrome (PTS) in which patients undergoing iliac vein stent placement are associated with postoperative early re-thrombosis [12]. In fact, other limited studies have shown that up to 40% of patients undergoing venous stenting may require additional recanalization to restore stent patency within the next 4 years [13, 14]. While our patient received both venous stent placement and anticoagulant therapy, recurrent DVTs and in-stent thrombosis continued to occur.
Despite the myriad of literature elucidating surgical approaches to MTS, there remains a paucity of studies analyzing effective anticoagulation therapies in MTS patient with recurrent thromboembolic events. In response, Birn and Vedantham have suggested that a more aggressive approach with both anticoagulation and anti-platelet therapy in the post-operative setting [12]. Some case reports have advocated for anticoagulant therapy for at least 6 months following stent placement for prevention of in-stent re-thrombosis [15]. A two-pronged strategy of DAPT in addition to anti-coagulation was successfully employed for prevention of recurrent thrombotic events including future in-stent, arterial, and venous thrombosis. MTS is a rare disease with limited guidelines. Given our case presentation, further investigations into the role of DAPT are warranted in patients with MTS and recurrent arterial and venous thromboses. Concurrently, establishment of guidelines for goal-directed therapy in primary and secondary prevention of recurrent thromboembolic events is prudent for patients with MTS prior to or after endovascular management.
This case highlights an unusual presentation of recurrent thromboembolic events including arterial thrombosis and recurrent DVTs in a young patient with MTS. Clinicians should consider MTS in the differential diagnosis of young adults presenting with left DVTs, especially in the face of recurrence, or other unprovoked thromboembolic events. DAPT is emerging as a therapy for secondary prevention of recurrent thrombotic events including recurrent in-stent thrombosis and arterial thrombosis. Future studies should focus on accurately measuring the incidence and prevalence of MTS and discovering efficacious medical therapies.
Conflict of Interest
None declared.
| References | ▴Top |
- May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8(5):419-427.
doi pubmed - Cockett FB, Thomas ML. The iliac compression syndrome. Br J Surg. 1965;52(10):816-821.
doi - O'Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, Dake MD. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000;11(7):823-836.
doi - Oguzkurt L, Ozkan U, Tercan F, Koc Z. Ultrasonographic diagnosis of iliac vein compression (May-Thurner) syndrome. Diagn Interv Radiol. 2007;13(3):152-155.
pubmed - Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39(5):937-943.
doi pubmed - Kiernan TJ, Yan BP, Cubeddu RJ, Rengifo-Moreno P, Gupta V, Inglessis I, Ning M, et al. May-Thurner syndrome in patients with cryptogenic stroke and patent foramen ovale: an important clinical association. Stroke. 2009;40(4):1502-1504.
doi pubmed - Verhaeghe R. Iliac vein compression as an anatomical cause of thrombophilia: Cockett's syndrome revisited. Thromb Haemost. 1995;74(6):1398-1401.
pubmed - Kolbel T, Lindh M, Akesson M, Wasselius J, Gottsater A, Ivancev K. Chronic iliac vein occlusion: midterm results of endovascular recanalization. J Endovasc Ther. 2009;16(4):483-491.
doi pubmed - Brazeau NF, Harvey HB, Pinto EG, Deipolyi A, Hesketh RL, Oklu R. May-Thurner syndrome: diagnosis and management. Vasa. 2013;42(2):96-105.
doi pubmed - Boc A, Boc V, Kozak M. May-Thurner syndrome: old acquaintance, new perspective : Case report. Wien Klin Wochenschr. 2017;129(9-10):362-365.
doi pubmed - Peters M, Syed RK, Katz M, Moscona J, Press C, Nijjar V, Bisharat M, et al. May-Thurner syndrome: a not so uncommon cause of a common condition. Proc (Bayl Univ Med Cent). 2012;25(3):231-233.
doi - Birn J, Vedantham S. May-Thurner syndrome and other obstructive iliac vein lesions: meaning, myth, and mystery. Vasc Med. 2015;20(1):74-83.
doi pubmed - Neglen P, Hollis KC, Olivier J, Raju S. Stenting of the venous outflow in chronic venous disease: long-term stent-related outcome, clinical, and hemodynamic result. J Vasc Surg. 2007;46(5):979-990.
doi pubmed - Raju S, Neglen P. Percutaneous recanalization of total occlusions of the iliac vein. J Vasc Surg. 2009;50(2):360-368.
doi pubmed - Kalu S, Shah P, Natarajan A, Nwankwo N, Mustafa U, Hussain N. May-thurner syndrome: a case report and review of the literature. Case Rep Vasc Med. 2013;2013:740182.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


