| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Original Article
Volume 7, Number 2, May 2018, pages 57-61
Prevalence of Anemia in Type 2 Diabetic Patients
Salma M. AlDallala, c, Nirupama Jenab
aHaematology Laboratory, Amiri Hospital, Kuwait
bDepartment of Biochemistry, Amiri Hospital, Kuwait
cCorresponding Author: Salma M. AlDallal, Haematology Laboratory, Amiri Hospital, Kuwait
Manuscript submitted April 17, 2018, accepted April 30, 2018
Short title: Anemia in Type 2 Diabetic Patients
doi: https://doi.org/10.14740/jh411w
| Abstract | ▴Top |
Background: The aim of the study was to determine the prevalence of anemia in patients with type 2 diabetes and to assess the risk of anemia according to gender, age and glycemic control.
Methods: The study group comprised of patients with type 2 diabetes attending Outpatient Diabetic Department of Amiri Hospital (Al-Asimah Capital area) from January 1, 2016 to December 31, 2017. Patients were divided into groups according to glycemic status and gender. Glycated hemoglobin (HbA1C) values and hemoglobin (Hb) levels were evaluated. The presence of anemia was defined by an Hb level < 13.0 g/dL for men and < 12.0 g/dL for women.
Results: The prevalence of anemia is significantly greater in diabetic females (38.5%) than in diabetic males (21.6%) and in poorly controlled diabetics (33.46%) than those with glycemic status under control (27.9%) (P < 0.05). The average age of patients with anemia was found to be 60.69 ± 0.198 years and the average age of patients without anemia was found to be 54.07 ± 0.121 years. This indicates that the risk of anemia increases with age.
Conclusion: Screening for anemia at the time of diagnosis of diabetes, diabetic medication compliance, awareness of the risk of anemia and other complications in the diabetic patients helps in reducing the prevalence of anemia in diabetic population.
Keywords: Type 2 diabetes; Anemia; Prevalence; Age; Gender; Glycemic status
| Introduction | ▴Top |
Anemia, as defined by World Health Organization (WHO) criteria less than 130 g/L for men and less than 120 g/L for women, is a common blood disorder [1, 2] and it is a condition in which the number of red blood cells (RBCs) is inadequate to meet the physiologic needs of the human body [3]. According to WHO, around half of the cases of anemia in the world are due to iron deficiency anemia (IDA) [4]. The reports showed that the prevalence of IDA is 2.5 times that of anemia [5]. In Kuwait, it is estimated that the prevalence of anemia is 3% in adult males and 17% in females [5].
Diabetes mellitus is one of the major causes of morbidity and mortality worldwide [6]. Worldwide prevalence of diabetes mellitus is 8.3% affecting approximately 382 million people. In Kuwait, the prevalence of type 1 diabetes is 2.8% among expatriates and 2.3% among natives in the age group of 0 - 20 years. Asian expatriates of the age group 30 - 60 years exhibit higher prevalence of type 2 diabetes than natives at 25.4% [7].
Diabetes mellitus can be classified into two types based on the insulin dependence. Type 1 diabetes mellitus is also known as juvenile diabetes or insulin-dependent diabetes, resulting from autoimmune destruction of insulin producing beta cells of pancreas. Whereas non-insulin-dependent diabetes, i.e. type 2 diabetes mellitus, results from insulin resistance. This is commonly seen in adults. Another type of diabetes, known as gestational diabetes, can develop during pregnancy, which improves or disappears after delivery, but studies showed that 20-50% cases of these can develop type 2 diabetes later in life [8].
Patients with type 2 diabetes mellitus are twice more likely to be prone to anemia than the patients without diabetes [9]. Bosman et al (2001) identified anemia as a risk factor for cardiovascular and end-stage renal diseases in diabetic patients [10]. Keane and Lyle (2003) [11] further proved that reduced hemoglobin (Hb) level identifies diabetic patients at increased risk for hospitalization and premature death. Despite these facts, anemia is unrecognized in 25% of the diabetic patients [12]. Recent studies have shown that the incidence of anemia in patients with diabetes is mostly associated with the presence of renal insufficiency. Thus, diabetic patients have a greater degree of anemia for their level of renal impairment than non-diabetic patients presenting with other causes of renal failure [1, 10, 13-15].
Factors suggested as the reason for the earlier onset of anemia in diabetic patients include systemic inflammation, inhibition of erythropoietin release, damage to the renal interstitium, severe symptomatic autonomic neuropathy causing efferent sympathetic denervation of the kidney and loss of appropriate erythropoietin, drugs, altered iron metabolism and hyper glycemia [16].
Some studies have shown that the diabetic patients with renal insufficiency are at a higher risk of developing anemia than normal diabetics as the ability of their kidneys to produce erythropoietin reduces. Also, the hormone responsible for the production of RBCs is affected by diabetic neuropathy resulting in anemia [2, 17, 18]. Subjects with diabetes also have nutritional deficiencies for cyanocobalamin, folate and iron which may result in different types of anemia. Metformin may interfere with cyanocobalamin absorption, resulting in vitamin B12 deficiency anemia [19, 20]. Because of the fact that both anemia and type 2 diabetes share similar symptoms like pale skin, chest pain, numbness or coldness in the extremities, shortness of breath and headache [20], anemia remains unidentified in most of the diabetes patients. Hence, it is important to identify anemia in the diabetic patients.
To estimate the prevalence of anemia in patients with type 2 diabetes mellitus in one Capital area of Kuwait, we analyzed data from laboratory information system (LIS) for adult patients attending Diabetes Outpatient Department (OPD) during January 2016 - December 2017. Data were analyzed according to gender, age and HbA1C status.
| Materials and Methods | ▴Top |
This was a retrospective study of patients attending OPD of Amiri Hospital (Al-Asima Capital area) and polyclinics, Kuwait. Data were collected from LIS with the approval of Health Center’s ethics committee.
Subjects
The study includes adult male and female patients with type 2 diabetes mellitus. Patients were divided into groups according to: 1) glycemic status, i.e. those with well controlled diabetes whose HbA1C level was equal to or less than 7.5% and poorly controlled diabetic group comprising those whose HbA1C level was greater than 7.5%; 2) gender, i.e. male and female; 3) presence of anemia which was considered as per the WHO gender specific criteria, i.e. less than 13 g/dL in men and less than 12 g/dL in women [16].
Data collection
Data of the study subjects were collected for a time period of 2 years between January 1, 2016 and December 31, 2017. From each case record, the information was collected under the following headings: age, gender, Hb value, and HbA1C value.
Exclusion criteria
Patients with type 1 diabetes mellitus were excluded.
Statistical analysis
Descriptive analysis was used to characterize the study sample by demographics, including gender, age, anemia and HbA1C level. Statistical analysis was performed using SPSS version 20.0. Significance was set as P < 0.05.
| Results | ▴Top |
This retrospective observational study was conducted at the OPD of Amiri Hospital (Al-Asima Capital area) and polyclinics, Kuwait. A total of 19,059 patients were included in the study, of which 9,957 were males and 9,102 were females (Table 1).
 Click to view | Table 1. Demographic Profile of the Patients |
The average age of patients with anemia was found to be 60.69 ± 0.198 years. The average age of patients without anemia was found to be 54.07 ± 0.121 years. The difference in the average age was statistically significant in the patients with anemia and without anemia (P < 0.05). This indicates that the risk of anemia increases with age.
Among these 19,059 patients, 5,655 patients were found to be anemic accounting for 29.7% prevalence of anemia in this population; 21.6% of diabetic males and 38.5% of diabetic females were found to be anemic.
Of these 19,059 patients, 13,038 had their diabetes under control, whereas 6,021 patients were poorly controlled diabetics; 27.9% patients of the well controlled diabetic group had anemia, whereas 33.46% patients of poorly controlled diabetic group had anemia (Fig. 1).
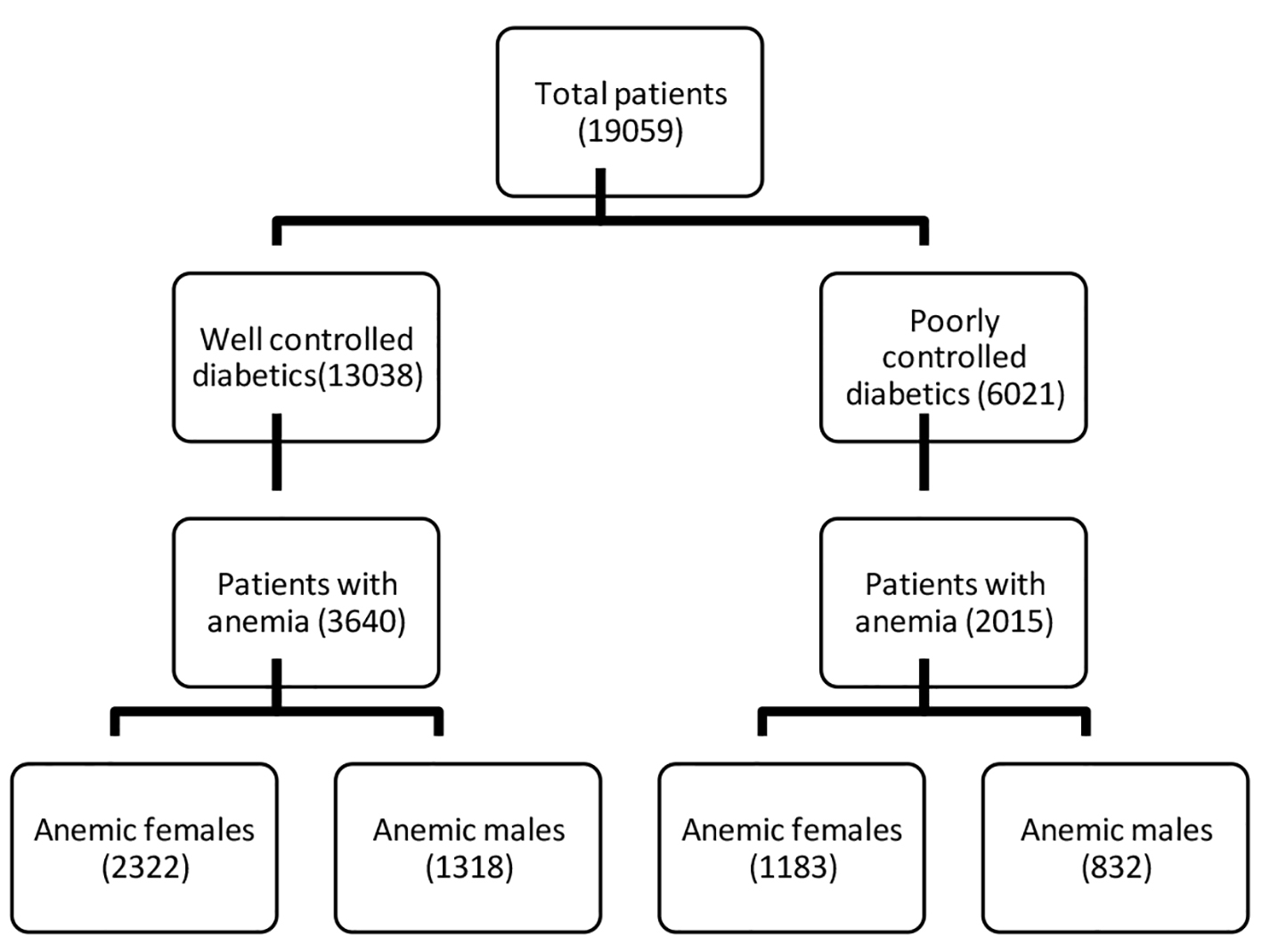 Click for large image | Figure 1. Categorization of patients according to presence of anemia based upon the diabetes control status. |
There is a statistically significant relation between prevalence of anemia and gender, i.e. the prevalence of anemia is significantly greater in diabetic females than diabetic males (P < 0.05). The prevalence of anemia is significantly greater in poorly controlled diabetics than those with glycemic status under control (P < 0.05) (Fig. 2).
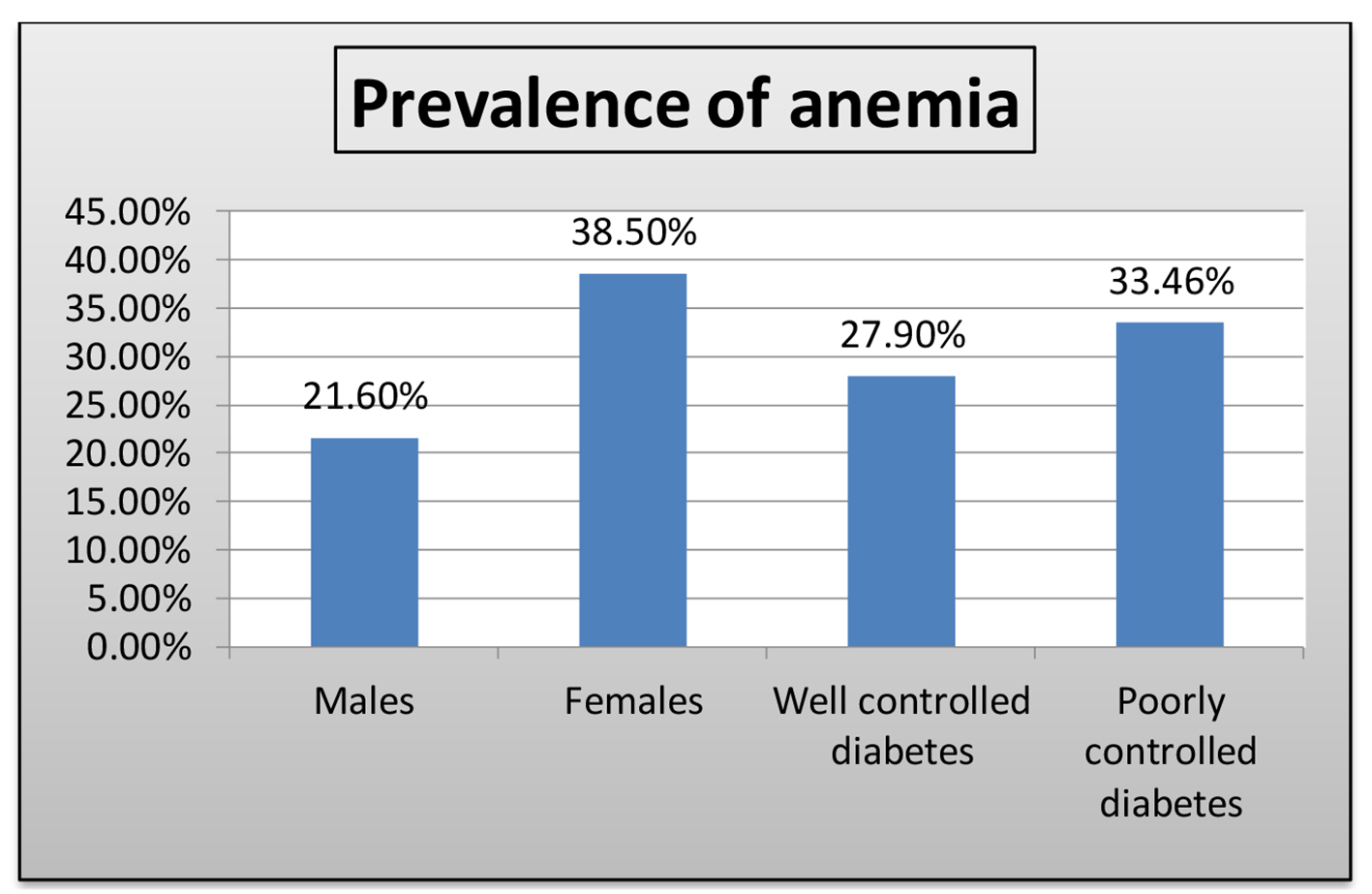 Click for large image | Figure 2. Prevalence of anemia according to gender and glycemic status in type 2 diabetic patients. |
| Discussion | ▴Top |
Patients with type 2 diabetes mellitus are twice more likely to be prone to anemia than the patients without diabetes. Bosman et al (2001) identified anemia as a risk factor for cardiovascular and end-stage renal diseases in diabetic patients [10]. Keane and Lyle (2003) [11] further proved that reduced Hb level identifies diabetic patients at increased risk for hospitalization and premature death. Despite these facts, anemia is unrecognized in 25% of the diabetic patients [12]. The current study estimated the prevalence of anemia in diabetic subjects and assessed the risk of anemia according to gender, age and glycemic control.
The prevalence of anemia in this study population was found to be 29.7% which is in contrast with the prevalence reported by Sharif et al (2014) which was 63% [6]. The huge difference in the prevalence of anemia might be due to the fact that population in this study were mostly poorly controlled diabetics (71.5%), whereas in the current study, 68% of the subjects are well controlled diabetics.
We found that diabetic females were at higher risk of anemia than diabetic males. This finding is consistent with the findings of Alsayegh et al (2017) which reported prevalence as 35.8% vs. 21.3% in diabetic females versus diabetic males [21]. The possible reason for higher prevalence of anemia in females might be due to poor nutrition, less importance given to their own health due to lack of empowerment. This can be improved by educational interventions such as health awareness programs in the rural areas, provision of iron rich food, prescription of vitamin and iron supplements and knowledge of the diabetic complications [22].
In our study, the prevalence of anemia is significantly higher in the poorly controlled diabetics. Also, the average age of the patients with anemia is significantly higher than average age of patients without anemia. These findings are in agreement with a recently published study by Mounika et al (2017) which reported poor glycemic control and old age to be associated with the higher incidence of anemia in diabetic patients [23]. Choi et al (2004) have also shown that the prevalence of anemia increases with the increasing age. The possible reasons for this increased prevalence with age might be due to deficiencies of vitamins such as folate, cyanocobalamin or bone marrow disorders and higher number of comorbidities [24]. In patients with poorly controlled diabetes, the erythrocyte precursors of the bone marrow might be prone to prolonged direct toxicity to glucose toxicity or the mature erythrocytes can be affected by oxidative stress leading to disturbances in the erythrocyte function [25].
Conclusion
This prospective observational study found a higher prevalence of anemia in diabetic females and patients with poorly controlled diabetes. Keeping the diabetes under control and proper investigations to identify anemia in diabetic patients at an early stage can reduce the severity of the complications caused due to anemia in diabetic population. Diabetic females and diabetic elderly are the most vulnerable group to anemia, thus care should be taken in terms of their nutrition and supplements. Physicians should be aware of the risk of anemia in these subgroups and should prescribe them with vitamin and iron supplements if required. Medication compliance must be achieved in the diabetic population in order to keep the glucose levels in the normal range. Awareness must be provided to the diabetic population at the time of their diagnosis of the risk of anemia and other complications of diabetes.
Acknowledgments
We would like to acknowledge Amiri Hospital (Al-Asima Capital area) and polyclinics, Kuwait for their kind cooperation in carrying out this study. The authors are thankful to www.manuscriptedit.com for providing English language editing and proofreading services for this manuscript. Special thanks to Mr. Gaurav Gyan Sharma (ATC, Kuwait) for helping in retrieving data from LIS.
Conflict of Interest
No conflict of interest is declared.
Abbreviations
WHO: World Health Organization; RBC: red blood cell; IDA: iron deficiency anemia; LIS: laboratory information system; HbA1C: glycated hemoglobin; Hb: hemoglobin
| References | ▴Top |
- Thomas MC, MacIsaac RJ, Tsalamandris C, Molyneaux L, Goubina I, Fulcher G, Yue D, et al. The burden of anaemia in type 2 diabetes and the role of nephropathy: a cross-sectional audit. Nephrol Dial Transplant. 2004;19(7):1792-1797.
doi pubmed - Adejumo BIG, Dimkpa U, Ewenighi C, Natuanya I. Incidence and risk of anemia in type-2 diabetic patients in the absence of renal impairment. Health Journal. 2012;4(6):304-308.
- Hemoglobin concentrations for the diagnosis of anemia and assessment of severity. Geneva: WHO. 2011.
- Iron deficiency anaemia: assessment, prevention and control, a guide for programme managers. Geneva: WHO, UNICEF, UNU. 2001.
- Al Zenki S, Alomirah H, Al Hooti S, Al Hamad N, Jackson RT, Rao A, Al Jahmah N, et al. Prevalence and determinants of anemia and iron deficiency in Kuwait. Int J Environ Res Public Health. 2015;12(8):9036-9045.
doi pubmed - Sharif A, Younus S, Baig K, Ali N. Prevalence and risk of anemia in type-2 diabetic patients. Health. 2014;6:1415-1419.
doi - Channanath AM, Farran B, Behbehani K, Thanaraj TA. State of diabetes, hypertension, and comorbidity in Kuwait: showcasing the trends as seen in native versus expatriate populations. Diabetes Care. 2013;36(6):e75.
doi pubmed - Johnson L, Gregory L, Christenson R, Harmening D. Appleton and lange series outline review clinical chemistry. New York: McGraw-Hill. 2001.
- Wright JA, Oddy MJ, Richards T. Presence and characterisation of anaemia in diabetic foot ulceration. Anemia. 2014;2014:104214.
doi pubmed - Bosman DR, Winkler AS, Marsden JT, Macdougall IC, Watkins PJ. Anemia with erythropoietin deficiency occurs early in diabetic nephropathy. Diabetes Care. 2001;24(3):495-499.
doi pubmed - Keane WF, Lyle PA. Recent advances in management of type 2 diabetes and nephropathy: lessons from the RENAAL study. Am J Kidney Dis. 2003;41(3 Suppl 1):S22-25.
doi pubmed - Abate A, Birhan W, Alemu A. Association of anemia and renal function test among diabetes mellitus patients attending Fenote Selam Hospital, West Gojam, Nowthwest Ethiopia: a cross sectional study. BMC Hematol, 2013;13(1):13-16.
doi pubmed - Dikow R, Schwenger V, Schomig M, Ritz E. How should we manage anaemia in patients with diabetes? Nephrol Dial Transplant. 2002;17(Suppl 1):67-72.
doi pubmed - Ishimura E, Nishizawa Y, Okuno S, Matsumoto N, Emoto M, Inaba M, Kawagishi T, et al. Diabetes mellitus increases the severity of anemia in non-dialyzed patients with renal failure. J Nephrol. 1998;11(2):83-86.
pubmed - El-Achkar TM, Ohmit SE, McCullough PA, Crook ED, Brown WW, Grimm R, Bakris GL, et al. Higher prevalence of anemia with diabetes mellitus in moderate kidney insufficiency: the kidney early evaluation program. Kidney Int. 2005;67(4):1483-1488.
doi pubmed - Craig KJ, Williams JD, Riley SG, Smith H, Owens DR, Worthing D, Cavill I, et al. Anemia and diabetes in the absence of nephropathy. Diabetes Care. 2005;28(5):1118-1123.
doi pubmed - Kojima K, Totsuka Y. Anemia due to reduced serum erythropoietin concentration in non-uremic diabetic patients. Diabetes Res Clin Pract. 1995;27(3):229-233.
doi - Ahmed AM, Hussein A, Ahmed NH. Diabetic autonomic neuropathy. Saudi Med J. 2000;21(11):1034-1037.
pubmed - Bolen S, Wilson L, Vassy J, et al. Agency for healthcare research and quality (US). Comparative effectiveness and safety of oral diabetes medications for adults with type 2 diabetes. 2011.
- Betcher B. Recognizing anemia in people with diabetes. 2009. Retrieved December 27, 2017, from Anemia Organization: www.anemia.org.
- Alsayegh F, Waheedi M, Bayoud T, Al Hubail A, Al-Refaei F, Sharma P. Anemia in diabetes: Experience of a single treatment center in Kuwait. Prim Care Diabetes. 2017;11(4):383-388.
doi pubmed - Rizvi N, Nishtar S. Pakistan's health policy: appropriateness and relevance to women's health needs. Health Policy. 2008;88(2-3):269-281.
doi pubmed - Mounika V, Sarumathy S, Ebens JA, Shanmugarajan TS. A prospective study on incidence of anaemia in type 2 diabetes mellitus patients. Research Journal of Pharmacy and Technology. 2017;10(1):11-14.
doi - Choi CW, Lee J, Park KH, Yoon SY, Choi IK, Oh SC, Seo JH, et al. Prevalence and characteristics of anemia in the elderly: cross-sectional study of three urban Korean population samples. Am J Hematol. 2004;77(1):26-30.
doi pubmed - Mahjoub AR, Patel E, Ali S, Webb K, Astrow A., Kalavar M. Anemia in diabetic patients without underlying nephropathy, a retrospective cohort study. 2016.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


