| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 1, Number 4-5, October 2012, pages 102-104
Megaloblastic Anaemia Presenting as Pyrexia: An Interesting Case Report
Deepak Jaina, c, Promil Jainb, HK Aggarwala, Vipin Kaverappaa, Ashwani Kumara
aDepartment of Medicine, Pt. B.D. Sharma University of Health Sciences, ROHTAK-124001 (Haryana), India
bDepartment of Pathology, Pt. B.D. Sharma University of Health Sciences, ROHTAK-124001 (Haryana), India
cCorresponding author: Deepak Jain, Department of Medicine, PGIMS, Rohtak-124001 (Haryana), India
Manuscript accepted for publication August 9, 2012
Short title: Megaloblastic Anaemia Presenting as Pyrexia
doi: https://doi.org/10.4021/jh40e
| Abstract | ▴Top |
Megaloblastic anemia is a rare cause of pyrexia. We report the case of a patient who presented with fever, anemia and thrombocytopenia. After ruling out infective, inflammatory and endocrine causes and correlating with vitamin B12 and folic acid levels, the cause was attributed to megaloblastic anemia. The patient responded well to the treatment with vitamin B12 and folic acid supplementation.
Keywords: Megaloblastic anemia; Pyrexia; Vitamin B12; Folic acid
| Introduction | ▴Top |
Vitamin B12 and folic Acid deficiency is a rare but treatable cause of fever of unknown cause that responds well to the treatment. Increased activity within bone marrow and defect in oxygenation to temperature regulatory area are proposed mechanisms. It should be considered in any patient who presents with pyrexia with pancytopenia.
| Case Report | ▴Top |
Thirty-six years old female, pure vegetarian since birth, having two children, of which youngest being 8 years old, presented with easy fatigability, dyspnoea on exertion for the last one and half month along with moderate to high grade fever for twenty days. The fever was continuous in nature, not associated with rigors and chills. There was no history of associated rash, cough and expectoration, headache, nausea, vomiting, any bowel and bladder disturbance, arthralgia, yellowness of sclera or altered sensorium. There was no significant past history or family history of any chronic illness like tuberculosis. Patient received intravenous ceftriaxone 1 g twice a day for seven days from a private practitioner but she did not respond. Her hematological investigations including complete hemogram revealed hemoglobin: 4.0 g%, WBC: 4,800/mm3 with Neutrophils 52% and Lymphocytes 48%, platelet count 50,000/mm3 and ESR 50 mm in first hour. Peripheral blood film was negative for malarial parasite. Urine complete examination was within normal limits with no pus cells on microscopy. As she did not respond to the treatment she was empirically put on anti-tubercular drugs and was referred to our hospital. Patient took anti tubercular treatment just for one day, and stopped it on her own.
At presentation, on physical examination, the patient was conscious, well oriented to time, place and person. Her pulse rate was 120/minute; regular, good volume with no radio-femoral delay, BP was 116/76 mmHg. The patient was febrile with temperature 40 °C and had marked pallor. The tongue was bald with loss of papilla. She had pale conjunctiva but there was no icterus, cyanosis, clubbing, lymphadenopathy, pedal edema rash or eschar or any peripheral stigmata of bacterial endocarditis. Oxygen saturation was 98% at room temperature with no signs of respiratory distress. Cardiovascular system revealed ejection systolic murmur in pulmonary area. Respiratory system and nervous system examination were essentially normal. Abdominal examination revealed mild hepatosplenomegaly with no ascites.
The patient’s complete haemogram revealed pancytopenia with an occasional hypersegmented neutrophil (value of complete haemogram at admission and during stay are shown in Table 1). The peripheral blood smear was suggestive of dimorphic anemia (Fig. 1). Biochemical examination including renal function tests and liver function tests were completely normal. Urine microscopy and gram’s stain were normal and urine culture was sterile. Repeated blood cultures were also found to sterile. Widal and Weil-felix tests were negative. Rapid Ag detection test for malaria and tests for Leptospira and ricketsial antibodies were also negative. Acetyl-choline esterase levels and chest radiograph were normal. Abdominal ultrasonography revealed mild hepatosplenomegaly but no lymphadenopathy. Her G6PD and Coombs tests were negative. Patient’s antinuclear antibodies, C-reactive protein and thyroid profile were normal. Her barium meal follow through & computed tomography scan (CT scan) of chest were unremarkable. As patient had low hemoglobin, investigations for anemia and bone marrow aspiration were contemplated. Bone marrow aspiration findings were suggestive of megaloblastic anemia with increased iron stores, without the presence of any granuloma or parasite (Fig. 2). On further evaluation her vitamin B12 levels were 100 pg/mL (normal 140 - 180 pg/mL) and folic acid levels were 3.8 mg%. Ferro-kinetic studies were normal.
 Click to view | Table 1. Serial Haemogram Before and After Treatment |
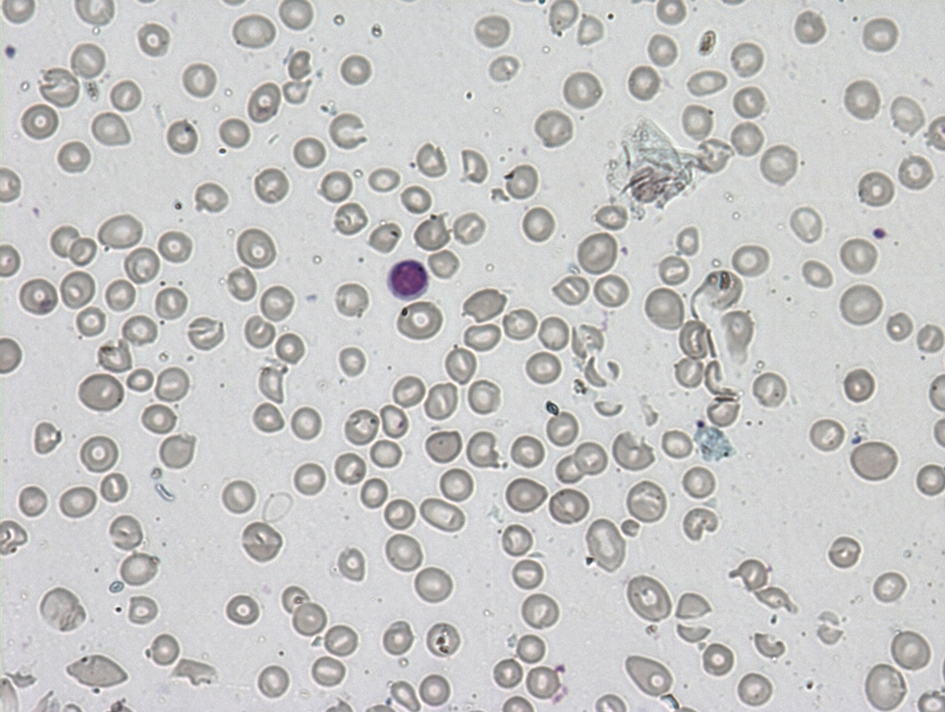 Click for large image | Figure 1. Peripheral blood smear showing dimorphic picture and pancytopenia. |
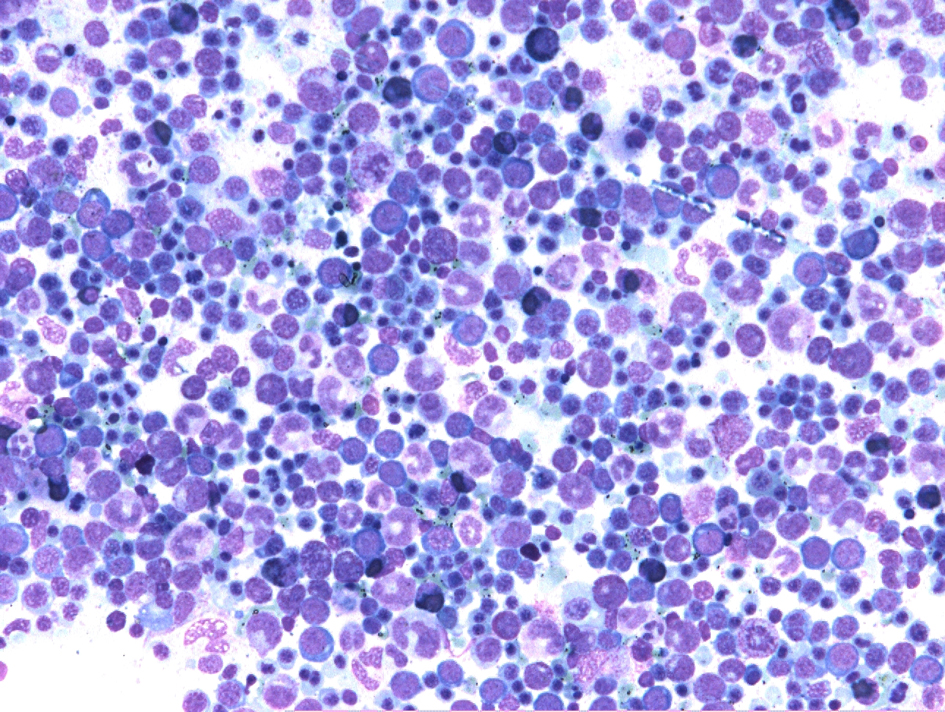 Click for large image | Figure 2. Bone marrow revealing megaloblastic erythropoiesis. |
On admission, patient was put on intravenous broad spectrum antibiotics with provisional diagnosis of pyrexia secondary to underlying sepsis of unknown origin. The patient continued to be febrile during stay at hospital. As she did not respond to antibiotics and there was absence of any positive findings, the antibiotics were stopped on seventh day of admission. After the reports of bone marrow aspiration were available, the patient was started on injectible cyanocobalamine 1,000 µg OD and folic acid 10 mg OD. Patient showed improvement 2 - 3 days after starting injection vitamin B12 and folic acid. She became completely afebrile on 5th day and remained so afterwards. Injection vitamin B12 along with folic acid was continued for 2 weeks. The patient showed marked improvement. Peripheral blood counts also improved thereafter. Subsequent measurement of vitamin B12 and folic acid at follow up showed normal values.
| Discussion | ▴Top |
Fever commonly occurs in megaloblastic anemia. Studies have shown that fever occurs in about 40% of patients with megaloblastic anemia caused by deficiency of either vit B12 or folic acid or both [1-3]. Usually this is low grade, high grade fever is seen in those patients who have more severe hematological disease [4, 5].
The exact cause of fever in megaloblastic anemia is still elusive and many hypothesis has been put forward in the past. The fever was previously attributed either to some defect in the temperature control mechanism of brain or to poor oxygenation of the temperature regulatory area secondary to vitamin B12 or folic acid deficiency [5-7]. Both these theories however fail to explain why the fever seen in megaloblastic anemia is not a recognized feature of other forms of anemia.
Megaloblastic bone marrow changes are associated with striking intramedullary hemolysis and possibly ineffective leukopoiesis and thrombopoiesis [1, 8]. Thus increased activity in bone marrow may be related to systemic pyrexia. The mechanism of how fever is induced by the overproduction marrow is not known [1]. The level of pyrexia usually correlates with degree of anemia and resolves very quickly after start of treatment. For those with high fever, 2 to 4 days are required for temperature to reach normal. In patients with folic acid deficiency there is a tendency for temperature to take slightly longer to drop below 37.8 °C [6, 9, 10]. Our case report also highlights this point and the improvement in fever is presumed to be due to improvement in bone marrow erythropoiesis.
Patients presenting with fever with pancytopenia are usually treated with broad spectrum antibiotics. However all these findings can be a part of megaloblastic anemia, which is rare, yet treatable cause of fever. Measurement of Vit B12 and folate levels should be considered in all patients of pyrexia with features of megaloblastic anemia and/or pancytopenia after ruling out infections, inflammatory and endocrine causes [1, 9]. However persistence of fever for several days or its failure to decrease even after 2 - 3 days of initiating vitamin B12 and folate therapy should suggest the possibility of another etiology for fever [1].
Conclusion
Megaloblastic anemia is rare but a known and treatable cause of fever. After ruling out infections and inflammatory conditions, which are important causes of fever in patients having pancytopenic picture, we should consider this possibility to be the etiological cause of fever. Easy availability and low cost of peripheral blood smear helps in screening these patients at an early stage. After measurement of vit B12 and folic acid levels, a trial of treatment based on these results can cause a rapid response and obviate the need further investigations and unnecessary antibiotic use.
Conflict of Interest
None.
| References | ▴Top |
- McKee LC, Jr. Fever in megaloblastic anemia. South Med J. 1979;72(11):1423-1424, 1428.
pubmed doi - Cabot RC. Pernicious and secondary anemia, chlorosis and leukemia. Modern medicine. Osler W, Mac CT (eds). Philadelphia. Lea and Febiger, Vol. IV. 1908.
- Gatenby PB, Lillie EW. Clinical analysis of 100 cases of severe megaloblastic anaemia of pregnancy. Br Med J. 1960;2(5206):1111-1114.
pubmed doi - Hoffbrand HV. Megaloblastic anemia and miscellaneous deficiency anemias. In: Worrell DA, Cox TM, Firth JD, Ben Jr, editor. Oxford Textbook of clinical Medicine. 4. Vol. 3. Oxford: Oxford University Press 2003: 659-75.
- Jones RV, Payne RW. The occurrence of fever in anemia. Practitioner.1960;184: 618-20.
- Singanayagam A, Gange N, Jones H. Folate deficiency presenting as pyrexia: a case report. Cases J. 2008;1(1):275.
pubmed - Davidson S. Clinical picture of pernicious anemia prior to introduction of liver therapy in 1929 and in Edinburgh subsequenuents to 1944. Lancet 1957;1:241-3.
- Perillie PE, Kaplan SS, Finch SC. Significance of changes in serum muramidase activity in megaloblastic anemia. N Engl J Med. 1967;277(1):10-12.
pubmed doi - Negi RC, Kumar J, Kumar V, Singh K, Bharti V, Gupta D, Kashyap R, et al. Vitamin B12 deficiency presenting as pyrexia. J Assoc Physicians India. 2011;59:379-380.
pubmed - Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 40-2000. A 38-year-old woman with gastric adenocarcinoma. N Engl J Med. 2000;343(26):1951-1958.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


