| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 8, Number 4, December 2019, pages 168-170
Serendipitous Finding of Asymptomatic Babesiosis in a Patient With Symptomatic Thrombocytopenia
Lalitha Ananda, Morana Vojnica, Colette Spaccaventoa, b
aDivision of Hematology/Oncology, Lenox Hill Hospital, New York, NY, USA
bCorresponding Author: Colette Spaccavento, Division of Hematology/Oncology, Lenox Hill Hospital, New York, NY, USA
Manuscript submitted October 15, 2019, accepted December 4, 2019
Short title: Asymptomatic Babesiosis With Thrombocytopenia
doi: https://doi.org/10.14740/jh570
| Abstract | ▴Top |
We report a case of isolated immune thrombocytopenic purpura (ITP) as a result of babesiosis infection. The patient initially presented with a history, physical exam and laboratory findings consistent with idiopathic thrombocytopenic purpura. She was treated with standard of care therapy without clinical response. Daily evaluation of the peripheral smear ultimately revealed a red blood cell inclusion, identified and confirmed as a low-titer babesiosis infection indicative of past exposure. As described below, isolated thrombocytopenia related to babesiosis infection has not been reported prior to the patient’s presentation. There are a few cases reported to show a relationship between babesiosis and autoimmune hemolytic anemia without an understood pathophysiologic mechanism. We review the literature, propose a possible pathophysiologic mechanism of disease and consider the implications of swift identification to prevent clinical deterioration.
Keywords: Babesiosis; Immune thrombocytopenic purpura; Isolated thrombocytopenia; Tick-borne illnesses
| Introduction | ▴Top |
Babesiosis is a common tick-borne infection endemic in Northeastern United States, affecting nearly 9-10% of the population in endemic areas [1]. The immunocompetent host typically clears the infection and may be asymptomatic or manifest only constitutional symptoms. However, in immunocompromised individuals or those post-splenectomy, a fulminant presentation including combined anemia and thrombocytopenia may occur [2-4].
Idiopathic or immune thrombocytopenic purpura (ITP) is an acquired thrombocytopenia caused by autoantibodies against platelet antigens. ITP can be primary, secondary, or drug-induced. Initial management includes steroids and intravenous immunoglobulin (IVIG) therapy followed by chemo-immunomodulators and splenectomy as second-line therapy. Testing for viral, bacterial and zoonotic infections is indicated in at-risk populations [5].
| Case Report | ▴Top |
A previously healthy 55-year-old woman presented to the emergency department with acute onset of petechiae and ecchymosis of the extremities progressively worsening over a course of 4 days. Review of systems was negative for fevers, chills, weight loss and trauma to the extremities, and notable for a remote tick bite without subsequent sequelae. On presentation, she was afebrile and normotensive with physical examination significant for diffuse scattered non-blanching petechiae and ecchymosis of the trunk, abdomen and extremities, a hemorrhagic bullous lesion of the buccal mucosa and without evidence of scleral icterus, conjunctival pallor or hepatosplenomegaly.
Initial diagnostic tests revealed severe thrombocytopenia (3.0 × 103) with otherwise normal complete blood count, complete metabolic panel, hemolysis studies and coagulation studies. The peripheral smear revealed thrombocytopenia without platelet clumping, rare atypical lymphocytes, normocytic normochromic red blood cells (RBCs) without evidence of schistocytes. Additional laboratory evaluation excluded infectious, nutritional deficiency and rheumatologic etiologies for thrombocytopenia. Imaging was negative for splenomegaly. The patient was diagnosed with ITP and treated with oral prednisone and IVIG resulting in a swift improvement of her platelet count in 3 days. She was discharged with a platelet count 33.0 × 106/µL, but re-admitted after 2 days with a headache and thrombocytopenia of 8.0 × 106/µL. A computed tomography (CT) of the head was negative for intracranial hemorrhage. A bone marrow biopsy (Fig. 1) obtained at this time was consistent with a diagnosis of ITP.
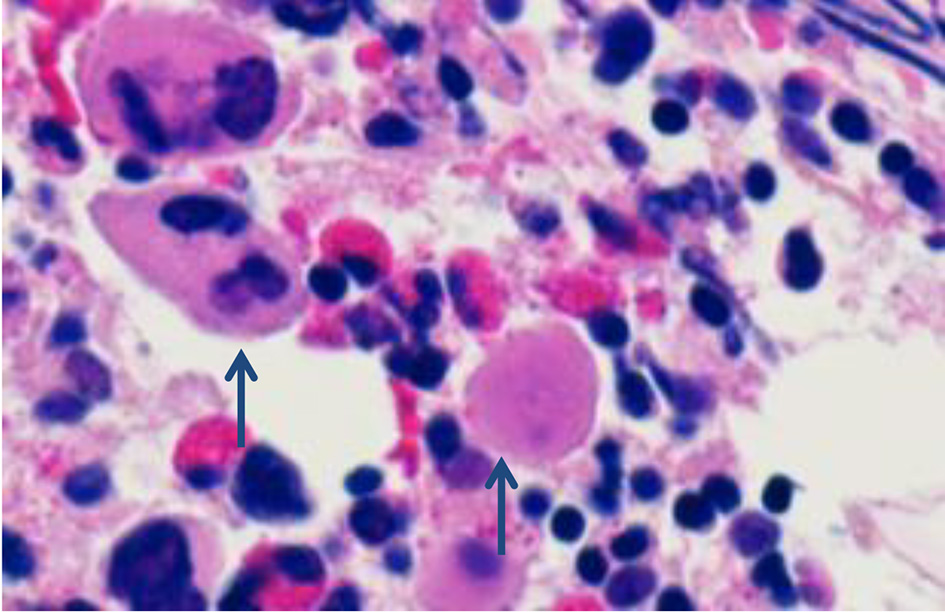 Click for large image | Figure 1. Bone marrow biopsy showing increased number of megakaryocytes that are atypical (high-power view, × 100/1.30 oil). |
She was re-challenged with IVIG and dexamethasone with a modest response in platelet count. All other labs were normal without evidence of hemolysis; however, a peripheral smear showed evidence of parasitic inclusions of the RBCs (Fig. 2) with 0.20% infection rate with babesia microti, confirmed by polymerase chain reaction (PCR).
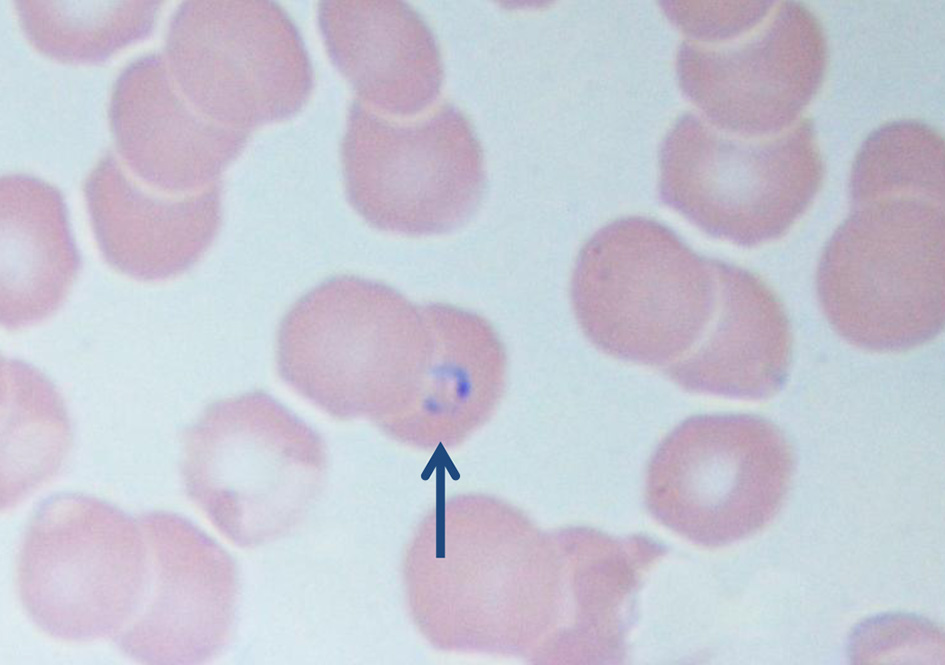 Click for large image | Figure 2. High-power view of peripheral smear showing intra-erythrocyte inclusion and absence of platelets (× 100/1.30 oil). |
Given the suboptimal response to initial standard management of ITP, she was started on azithromycin and atovaquone for management of babesiosis resulting in rapid improvement of platelet count (Fig. 3). The patient completed treatment for babesiosis as an outpatient and follow-up revealed a normal platelet count and clearance of the parasitemia.
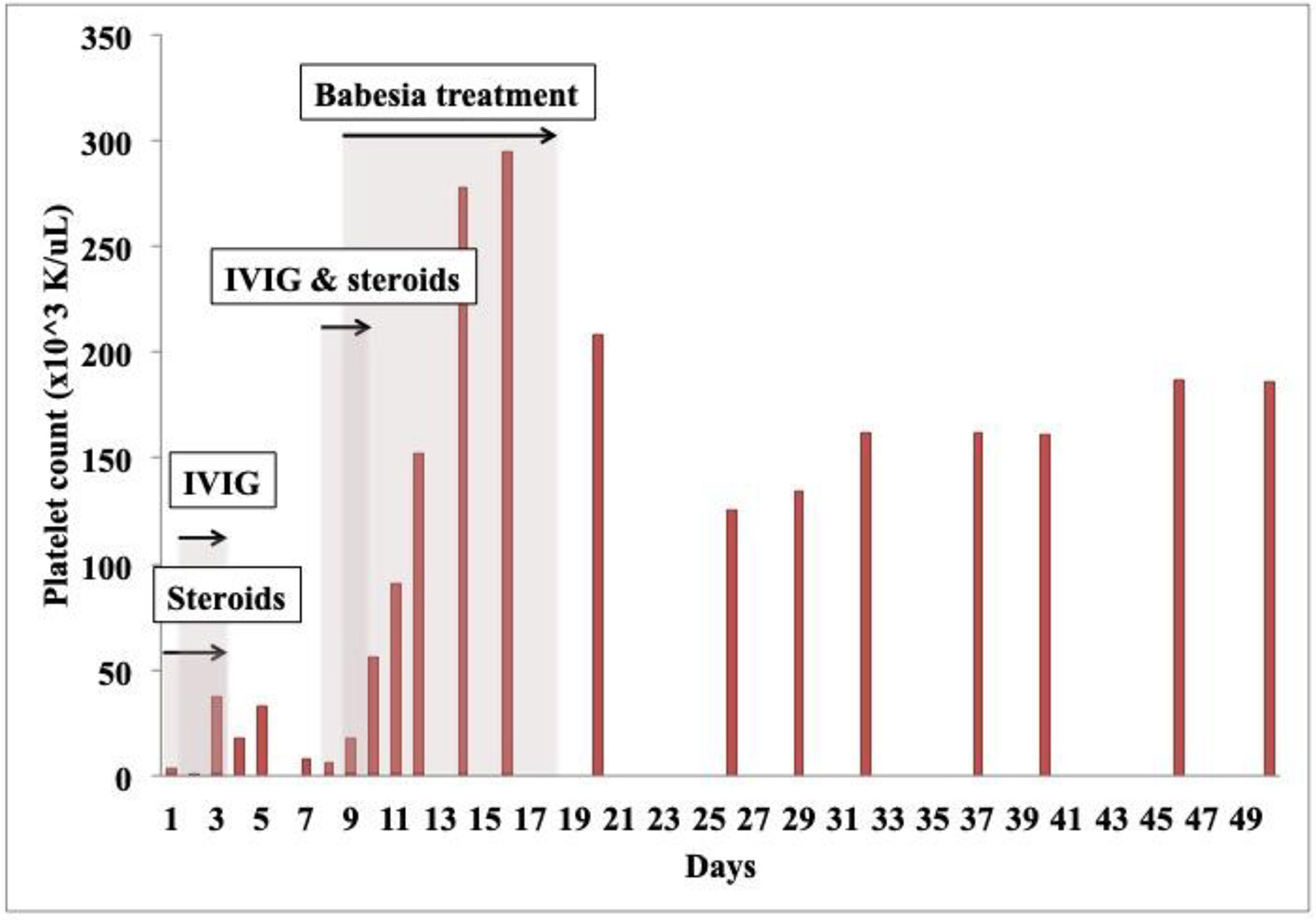 Click for large image | Figure 3. Platelet count change with various treatments. IVIG: intravenous immunoglobulin. |
| Discussion | ▴Top |
This case presents a previously underreported relationship between babesiosis and isolated thrombocytopenia [6]. This patient exhibited a partial response to immunosuppressive therapy seemingly enhanced by the addition of treatment for babesiosis indicating that the cause of thrombocytopenia was likely linked to the parasitemia. Though the pathophysiologic mechanism for babesiosis-induced isolated thrombocytopenia is still not clearly defined, a review of recent literature broadly categorizes the etiology as either immune or non-immune and immune-mediated [7, 8]. An immune or autoimmune phenomenon may be identified by flow cytometry to demonstrate presence of anti-platelet antibodies. Additionally, empiric management of ITP should result in improvement of thrombocytopenia. Babesiosis may trigger the complement immune system and result in hemophagocytic lymphohistiocytosis (HLH). Non-immune causes postulated include splenomegaly with associated peripheral destruction of platelets, splenic rupture, direct consumption and injury to the platelets, and marrow suppression [7, 8].
Splenomegaly with its associated peripheral destruction is the most likely cause of thrombocytopenia in tick-borne illnesses. Particularly in babesiosis, several cases have revealed severe splenomegaly with splenic rupture who also had thrombocytopenia [7]. Further analysis studying a database of infected individuals will likely help identify the pathophysiology behind isolated thrombocytopenia in babesiosis. Ultimately, it is paramount that the workup for presumed autoimmune thrombocytopenia includes evaluation for tick-borne illnesses, especially in the Northeastern United States, to facilitate swift medical management.
Learning points
1) Babesiosis, a clinically relevant disease to recognize in the Northeastern United States, has hematologic implications that necessitate swift diagnosis and intervention.
2) ITP is often idiopathic, but identifiable causes, including tick-borne illnesses, are important and will assist the clinician in choosing the appropriate therapy.
3) Common hematologic abnormalities seen in acute babesiosis infection include concurrent hemolytic anemia with thrombocytopenia, but isolated thrombocytopenia may be a presenting laboratory finding in chronic babesiosis.
4) The pathophysiologic mechanism of isolated thrombocytopenia in babesiosis infection is unknown and needs to be further studied.
Acknowledgments
Special thanks to Irina Gershman from the Hematology Laboratory at Lenox Hill Hospital for her contribution with evaluation of the peripheral smear.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
LA and MV wrote the manuscript; MV did the background research; CS provided the case, reviewed and amended the manuscript. All authors reviewed the final manuscript.
| References | ▴Top |
- Center for Disease Control: Surveillance for Babesiosis - United States, 2014; updated February 29, 2016.
- Shatzel JJ, Donohoe K, Chu NQ, Garratty G, Mody K, Bengtson EM, Dunbar NM. Profound autoimmune hemolysis and Evans syndrome in two asplenic patients with babesiosis. Transfusion. 2015;55(3):661-665.
doi pubmed - Herman JH, Ayache S, Olkowska D. Autoimmunity in transfusion babesiosis: a spectrum of clinical presentations. J Clin Apher. 2010;25(6):358-361.
doi pubmed - Evenson DA, Perry E, Kloster B, Hurley R, Stroncek DF. Therapeutic apheresis for babesiosis. J Clin Apher. 1998;13(1):32-36.
doi - Cines DB, Bussel JB. How I treat idiopathic thrombocytopenic purpura (ITP). Blood. 2005;106(7):2244-2251.
doi pubmed - Akel T, Mobarakai N. Hematologic manifestations of babesiosis. Ann Clin Microbiol Antimicrob. 2017;16(1):6.
doi pubmed - Narurkar R, Mamorska-Dyga A, Agarwal A, Nelson JC, Liu D. Babesiosis-associated immune thrombocytopenia. Stem Cell Investig. 2017;4:1.
doi pubmed - Woolley AE, Montgomery MW, Savage WJ, Achebe MO, Dunford K, Villeda S, Maguire JH, et al. Post-babesiosis warm autoimmune hemolytic anemia. N Engl J Med. 2017;376(10):939-946.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


