| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 2, Number 1, June 2013, pages 42-47
Unconventional Presentation of Multiple Myeloma: A Series of 4 Cases
Monika Guptaa, b, Mansi Kalaa, Sant Prakash Katariaa, Padam Parmara, Gajender Singha, Sunita Singha, Rajeev Sena
aDepartment of Pathology, Pt. BDS, PGIMS, University of Health Sciences, Rohtak, India
bCorresponding author: Monika Gupta, 17/8 FM, Medical Enclave, PGIMS, Rohtak, Haryana, India
Manuscript accepted for publication March 12, 2013
Short title: Unconventional Presentation of Multiple Myeloma
doi: https://doi.org/10.4021/jh73w
| Abstract | ▴Top |
Plasma cell neoplasm and related disorders are clonal proliferation of immunoglobulin producing plasma cells. Most plasma cell abnormality originates as bone marrow tumor, but they occasionally present in extra medullary sites. We report a series of four cases of multiple myeloma diagnosed at Tertiary care hospital. They presented as acute renal failure at young age, primary amyloidosis tongue, non-specific back pain and as extra medullary dissemination in pulmonary parenchyma. We have reported these cases in order to demonstrate the variability in the presentation of multiple myeloma. These uncommon presentation can easily be missed and give us insight for considering the possibility of multiple myeloma with uncommon findings.
Keywords: Multiple myeloma; Amyloidosis; Non-secretory; Acute renal failure
| Introduction | ▴Top |
Multiple myeloma (MM) is a clonal malignancy of terminally differentiated B lymphocytes characterized by uncontrolled proliferation of abnormal plasma cells. The clinical features of the disease may be directly due to proliferation process itself and or indirectly to substances released by the neoplastic cells. The former, results in bone marrow displacement with suppression of normal hematopoiesis and multiple osteolytic lesions with pathological fractures, while the later, results in the accumulation of monoclonal immunoglobulin’s (Igs) (heavy and light chain), osteoclast activating factor and other regulating substances. The circulating monoclonal Igs or their subunits are leading cause of proteinuria, renal tubular damage and amyloid deposits. Stimulation of osteoclasts may result in hypercalcemia and bone loss [1, 2].
The clinical manifestation of multiple myeloma depends on the site and extent of involvement. They have varied presentation, 10-40% cases being asymptomatic and 50-70% having bony pain due to lytic lesions and pathological fractures. About 1-5% cases may not demonstrate Igs or their subunits in serum or urine (non-secretory multiple myeloma) [3]. The occurrence of extramedullary disease is uncommon in multiple myeloma. Myeloma cells found at extramedullary site may either be due to extramedullary plasmacytoma (EMP), a variant of multiple myeloma or due to extramedullary dissemination of multiple myeloma. The sites of extramedullary dissemination reported in the literature are spleen, liver, kidney, thyroid, adrenal, ovary, lung, pleura, and pericardium [4]. We encountered four cases of multiple myeloma from July 2011 to Dec 2012 with uncommon presentation in our institute. Brief clinical summary of the cases is as follows.
| Case Report | ▴Top |
Case 1
A 50-year-old male presented with a vague complaint of chest pain, cough and mild breathlessness of 6 months duration. The pain was moderate in intensity and constant. Patient was nonsmoker, non-alcoholic with no history of fever or preceding trauma. Physical examination revealed no significant abnormality except mild pallor. Radio imaging of chest revealed large peripheral lung mass with smooth margins in lateral segment of right middle lobe showing homogenous contrast enhancement with erosion of the adjacent vertebra and ribs (Fig. 1). Routine investigations revealed normal blood counts with high sedimentation rate. There was no renal insufficiency and liver functions were within normal limits. Percutaneous fine needle aspiration cytology and biopsy from pulmonary lesion was done which showed cellular infiltrate comprising mature and immature plasma cells, including binucleate and multinucleate forms along with pulmonary parenchymal cells. Diagnosis of plasmacytoma was suggested and further work up of patient was advised to rule out pulmonary dissemination of multiple myeloma. A subsequent skull radiograph showed multiple punched out lytic lesions. Bone marrow aspiration revealed about 10% plasma cells. Serum protein electrophoresis showed a monoclonal spike in gamma region which on Immunofixation (IF) confirmed it as IgG kappa type monoclonal gammapathy. Bence Jones proteinuria was absent. A final diagnosis of multiple myeloma with dissemination in pulmonary parenchyma and adjoining soft tissues was made. Patient was put on chemotherapeutic agents like melphalan and prednisolone however, patient lost to follow up.
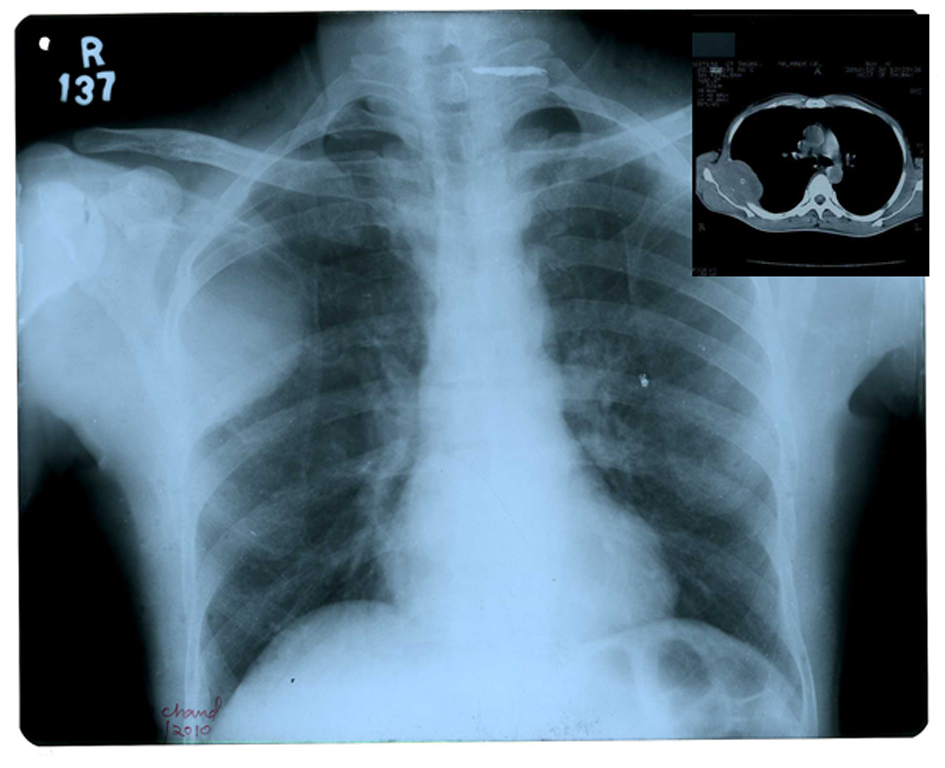 Click for large image | Figure 1. X-ray chest PA view showing a homogenous opacity in right middle lobe. Inset CT scan showing mass in right lung extending in thoracic cage. |
Case 2
A 70-year-old female presented with complaints of stiffness of tongue, difficulty in swallowing and weight loss. Initial examination revealed enlarged and firm tongue with limited mobility. The incisional biopsy of tongue revealed a hyperplastic epithelium, atrophic muscle fibers and perivascular amorphous, hyaline, eosinophilic substance on H&E staining (Fig. 2). Congo red stain performed showed orange color to the tissue deposit which reacted positively with anti-amyloid kappa. A provisional diagnosis of primary amyloidosis of the tongue was considered and further laboratory examination was performed. Investigations revealed normal blood counts with high sedimentation rate. Other biochemical results were within normal limits. Bone marrow aspiration revealed 60% of mature and immature plasma cells. Radiographic studies showed multiple lytic lesions in the skull, humerus and ribs. Serum protein electrophoresis evaluated normal serum proteins. The urine was positive for Bence Jones proteins. Urine protein electrophoresis (total protein, 3,000 mg/24 hours), demonstrates a single M protein peak in the gamma region which on urine immunofixation electrophoresis confirmed it as monoclonal free kappa light chains. The diagnosis of multiple myeloma with secondary amyloidosis tongue was made. Patient was referred to hematology for chemotherapy.
 Click for large image | Figure 2. Tongue showing macroglossia. Inset biopsy tongue showing hyperplastic epithelium, atrophic muscle fibres and hyaline eosinophilic substance (H&E stain × 200). |
Case 3
A 38-year-old male presented to emergency care with complains of abdominal cramps associated with nausea, vomiting, and decreased appetite. He revealed past history of intermittent low-grade fever without chills and rigors and nonspecific pain in his back and knee joints for which he was taking non-steroidal anti-inflammatory medicines along with physiotherapy. There was no history of weight loss, diarrhoea, or night sweats. Physical examination revealed only mild discomfort on deep palpation of abdomen. Supportive treatment was initiated and routine investigations were done. Investigations revealed normal blood counts with renal insufficiency (blood urea 103 mg/dL, serum creatinine 15.0 mg/dL). The serum calcium level and total protein were within normal limits. Urine analysis showed mild proteinuria, hematuria and granular casts. Since the etiology of the patient’s renal failure was not clear, a percutaneous renal biopsy was performed. Light microscopy revealed deposits of eosinophilic hyaline substance in the mesangial matrix and around blood vessels of glomeruli which was positive for Congo red stain (Fig. 3). Initial diagnosis of renal amyloidosis was made. Further investigation like serum protein electrophoresis revealed a monoclonal spike in the gamma region, which on serum immunofixation electrophoresis confirmed it as IgG kappa monoclonal gammapathy (Fig. 4). Radio imaging showed lytic lesions in skull, vertebrae and femur. The aspirated bone marrow revealed 40% abnormal plasma cells confirming the diagnosis of multiple myeloma with renal amyloidosis. The chemotherapy was initiated with bortezomib infusions and dexamethasone. The patient had excellent response to chemotherapy as his serum creatinine began to improve.
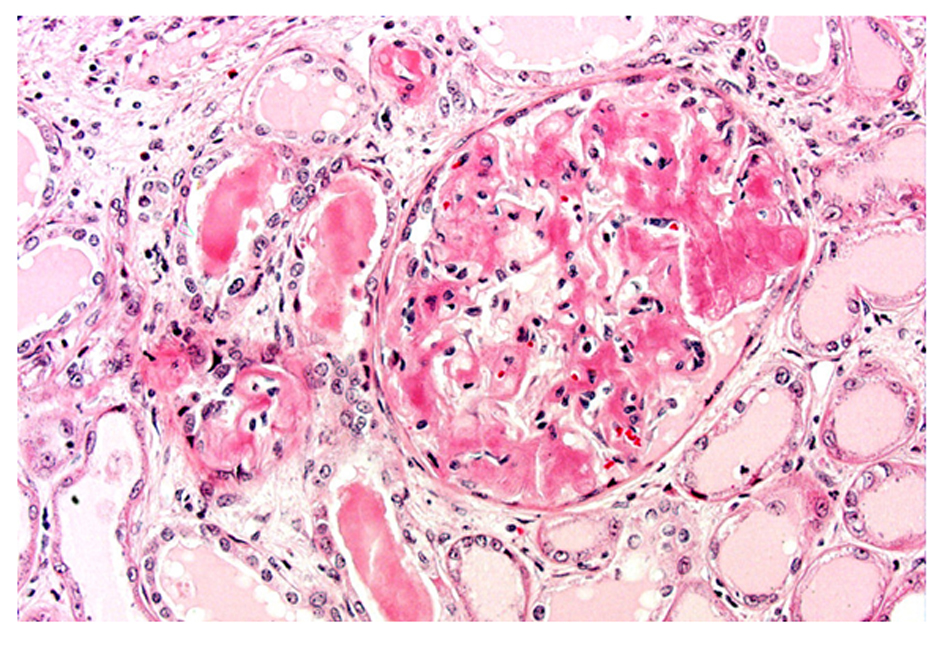 Click for large image | Figure 3. Renal biopsy showing obliteration of glomerular architecture by accumulation of amyloid and eosinophilic hyaline cast in tubules (PAS stain × 200). |
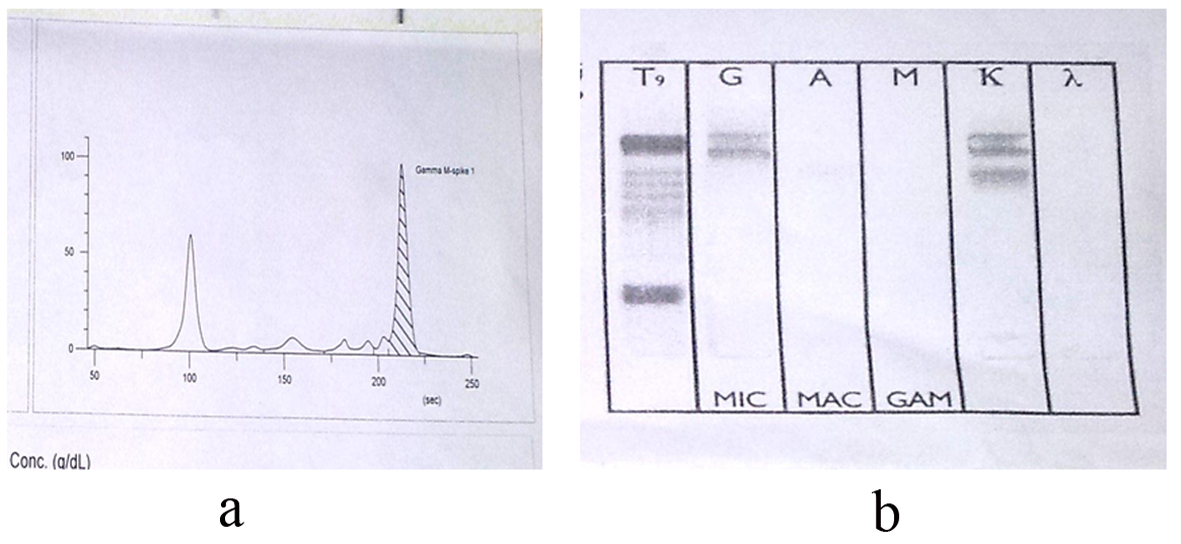 Click for large image | Figure 4. a). Serum Protein Electrophoresis showing “M” Spike in gamma globulin region. b). Serum Immunofixation Electrophoresis (IFE) identified the “M” spike as IgG and Kappa. |
Case 4
A 53-year-old female presented with complaints of back ache and right knee joint pain of two year duration. There was no history of trauma or history suggestive of any significant relation to backache and joint pain. Examination revealed tenderness on the right side of the thoracolumbar spine along with paravertebral muscle spasm. Bilateral hip joints were clinically normal with no joint movement restriction. Neurological examination showed no root stretch signs or neurological deficit. Laboratory evaluation revealed mild anemia with normal sedimentation rate. Biochemical work up was with in normal limits. Radio imaging revealed collapse and compression fracture of T9 vertebrae (Fig. 5). There was no relief from pain with the symptomatic treatment. A subsequent bone scan showed abnormal increase uptake in thoracolumbar vertebrae, multiple bilateral ribs and right iliac bone. Serum protein electrophoresis was normal. There was no Bence Jones protein in urine. In view of the bony pain with radiological findings, normal myeloma screen, normal calcium levels and abnormal bone scan findings, bone marrow aspiration was performed which revealed a hypercellular marrow with near total replacement by mature and immature plasma cells (80%) (Fig. 6). Diagnosis of non-secretory multiple myeloma was made. Patient received radiation to relieve his back pain followed by chemotherapy (Table 1).
 Click for large image | Figure 5. CT thoracic spine: sagittal view-showing multiple punched out lytic lesions in vertebral bodies and compression fracture of T9 vertebral body (arrow). |
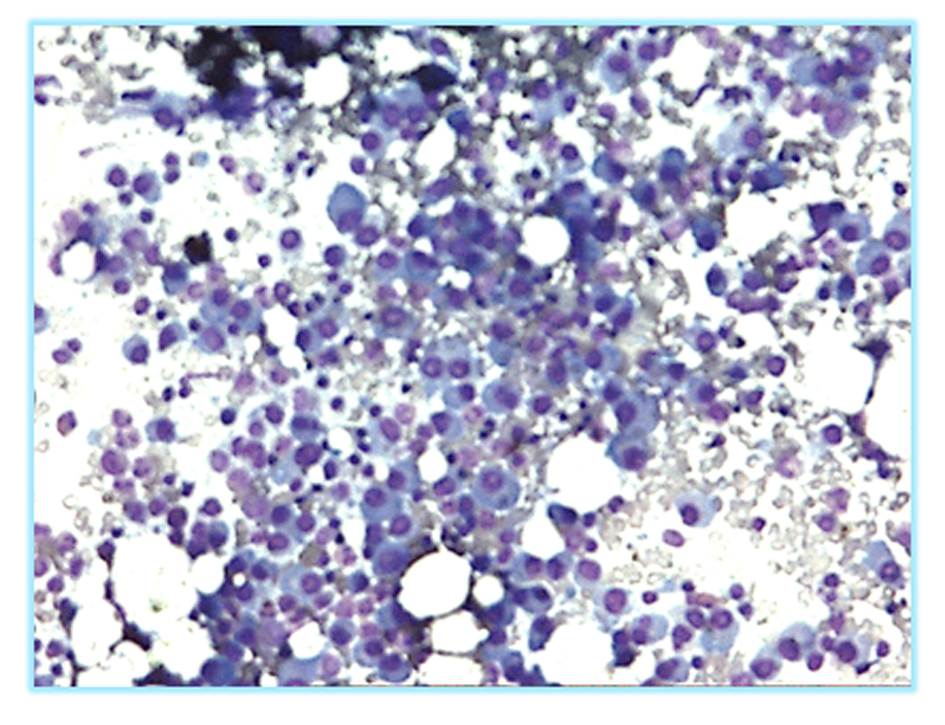 Click for large image | Figure 6. Bone marrow aspirate showing plasmacytosis (Leishman stain × 200). |
 Click to view | Table 1. Clinical Details of the Patients |
| Discussion | ▴Top |
Multiple myeloma is a clonal proliferation of plasma cells that occurs in older adults, median age at diagnosis is about 70 years [5, 6]. Presenting symptoms are variable, including fatigue, generalized weakness, weight loss, and bone pain, and there is often evidence of some organ damage [7]. The diagnosis of multiple myeloma depends on a concurrence of features, and several different diagnostic criteria as suggested by the International Myeloma working group [8].
Bone pain, the most common presenting symptom, occurs in approximately two-thirds of patients. The pain is caused by lytic bone lesions as a result of excess osteoclast activation and suppression of osteoblasts mediated by the malignant cells. They also have an increased risk of vertebral compression fractures [9]. Three of our patients presented with nonspecific pain in chest, back and knee joint with no improvement with symptomatic treatment. Typically, pain of pathological origin should be suspected in patient’s age over 50, a previous history of cancer, no relief with rest, resistant to treatment and constitutional symptoms such as unexpected weight loss, fever, and fatigue [10]. Differential diagnosis includes metastatic tumors, lymphomas, primary bone lesions and other lesions of hematopoietic origin such as langerhan’s cell histiocytosis [11]. Radiographic evaluation should always be persuaded in patients with pain.
Amyloidosis is reported in 6-15% of patients with multiple myeloma as an additional complication. Oral manifestation is common in primary amyloidosis but rarely oral amyloidosis may be the first symptom of multiple myeloma [12]. In the second case, the female presented with weight loss and macroglossia. Causes of macroglossia include hypothyroidism, lymphoma, hemangioma, neurofibroma, Down syndrome, acromegaly and amyloidosis [13]. These lesions may interfere with speech, chewing, swallowing as was seen in our case. As multiple myeloma evaluated as a grave factor, a complete work up of plasma cell dyscrasias should be performed especially in older patients presenting with primary amyloidosis.
Usually 15% to 30% of patients of multiple myeloma present with acute renal failure at the time of diagnosis and approximately 20% of the patient develops progressive renal failure during the course of the disease [14]. The pathophysiology of renal failure is often multifactorial and causes include the presence of excess myeloma protein, hypercalcemia as a result of excess osteoclast activity in the bones, dehydration, infection, and the use of NSAIDs for bone pain. Renal disease is more common in patients who produce excess light chains that get filtered through the glomeruli but then accumulate in the tubules. Renal function returns to normal after treatment in about 50% of patients [15]. In our case 3, young male presented with acute renal failure with no evidence of anemia or hypercalcemia despite numerous destructive bone lesion, made it a rare presentation of multiple myeloma. Multiple myeloma should always be considered in differential diagnosis of unexplained ARF in middle aged and elderly persons [16].
Rarely in advanced multiple myeloma, metastatic deposits outside the bone marrow (extramedullary) are seen. Multiple myeloma masquerading as pulmonary nodule is extremely rare and associated with aggressive terminal phase of myeloma [17]. Pulmonary involvement in myeloma is so rare that there is no mention of its occurrence even in a large series of 869 cases [18, 19]. In our patient after encountering atypical plasma cells in lung parenchyma we first investigated in order to find out whether he was having EMP or multiple myeloma with extra medullary dissemination. Since the treatment and prognosis of these two conditions are vastly different.
Since all our patients did not have any typical feature of multiple myeloma, highlights the importance of extensive evaluation of the patients. Variable presentation makes it difficult to provide a list of symptoms that are highly sensitive or specific to confirm or rule out the diagnosis of multiple myeloma.
Conclusion
The signs and symptoms of multiple myeloma are nonspecific. Patients can present in a variety of clinical settings, which may delay the diagnosis and result in additional disease related complications. We want to bring the clinicians attention to some uncommon presentations of multiple myeloma which are missed because of few unconventional findings.
| References | ▴Top |
- Raubenheimer EJ, Lello GE, Dauth J, Fayman MS, Dvornak N, Senekal JC. Multiple myeloma presenting as localized expansile jaw tumour. Int J Oral Maxillofac Surg. 1988;17(6):382-385.
doi - Bahlis NJ, Lazarus HM. Multiple myeloma-associated AL amyloidosis: is a distinctive therapeutic approach warranted? Bone Marrow Transplant. 2006;38(1):7-15.
doi pubmed - Middela S, Kanse P. Nonsecretory multiple myeloma. Indian J Orthop. 2009;43(4):408-411.
doi pubmed - Duggal RK, Ramachandran KA. Multipe myeloma with extramedullary dissemination in the lung. JIACM 2002;3:93-95.
- Wisloff F, Andersen P, Andersson TR, Brandt E, Eika C, Fjaestad K, Ly B, et al. Has the incidence of multiple myeloma in old age been underestimated? The myeloma project of health region I in Norway. I. Eur J Haematol. 1991;47(5):333-337.
doi pubmed - Bergsagel D. The incidence and epidemiology of plasma cell neoplasms. Stem Cells. 1995;13(Suppl 2):1-9.
- Kuo VC, Fenves AZ, Mehta AN. Multiple myeloma presenting as acute renal failure. Proc (Bayl Univ Med Cent). 2011;24(4):302-305.
- Kyle RA, Child JA, Anderson K, Barlogie B, Bataille R, Bensinger W et al. The international myeloma working group. Criteria for the classification of monoclonal gammapathies, multiple myeloma and related disorders: A report of the International Myeloma working group. Br J Haematol 2003;121:749-757.
doi - Agaja SB, Babalola OM, Olawumi HO, Babatunde AS. Unusual presentation of multiple myeloma: case report and review with focus on therapeutic and psychological aspects. The Internet Journal of Orthopedic Surgery 2007;6(2).
doi - Southerst D, Dufton J, Stern P. Multiple Myeloma presenting as sacroiliac joint pain: a case report. J Can Chiropr Assoc. 2012;56(2):94-101.
pubmed - Dauth J, de Coning JP, Politzer WM, Robertson T, Raubenheimer EJ. Unusual presentation of multiple myeloma. A report of 2 cases. S Afr Med J. 1984;65(24):968-971.
pubmed - Shibata M, Kodani I, Doi R, Takubo K, Kidani K, Sakai H et al. Multiple myeloma presenting symptoms in the oral and maxillofacial region. Yonago Acta Medica 2003;46:77-81.
- Sanli H, Ekmekci P, Terzi E, Erdem C. A case of multiple myeloma and amyloidosis of the tongue. Journal of Ankara Medical School. 2002;24:194-200.
- Goldschmidt H, Lannert H, Bommer J, Ho AD. Multiple myeloma and renal failure. Nephrol Dial Transplant. 2000;15(3):301-304.
doi pubmed - Vickrey E. Multiple myeloma: vague symptoms can challenge diagnostic skills. JAAPA. 2008;21(11):19-22.
doi pubmed - Prakash J, Niwas SS, Parekh A, Vohra R, Wani IA, Sharma N, Usha. Multiple myeloma—presenting as acute kidney injury. J Assoc Physicians India. 2009;57:23-26.
- Singh S, Jain P, Kala M, Sen R. Multiple myeloma masquerading as a pulmonary mass: A rare presentation. Dicle Med J 2012;39:110-113.
doi - Kintzer JS, Jr., Rosenow EC, 3rd, Kyle RA. Thoracic and pulmonary abnormalities in multiple myeloma. A review of 958 cases. Arch Intern Med. 1978;138(5):727-730.
doi pubmed - Muller AM, Geibel A, Neumann HP, Kuhnemund A, Schmitt-Graff A, Bohm J, Engelhardt M. Primary (AL) amyloidosis in plasma cell disorders. Oncologist. 2006;11(7):824-830.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


