| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 4, Number 1, March 2015, pages 137-140
Quinine-Induced Thrombocytopenia in a Patient With Myocardial Infarction
Ariela Marshalla, Rachel Rosovskyb, c
aDepartment of Hematology and Medical Oncology, Dana-Farber Cancer Institute, 450 Brookline Avenue, Smith 353, Boston, MA 02215, USA
bDepartment of Hematology and Medical Oncology, Massachusetts General Hospital, 55 Fruit Street, Boston, MA 02114, USA
cCorresponding Author: Rachel Rosovsky, Department of Hematology and Medical Oncology, Massachusetts General Hospital, 55 Fruit Street, Boston, MA 02114, USA
Manuscript accepted for publication August 15, 2014
Short title: Quinine-Induced Thrombocytopenia
doi: http://dx.doi.org/10.14740/jh92w
| Abstract | ▴Top |
Quinine-induced thrombocytopenia is a relatively rare phenomenon likely mediated by both quinine-induced production of anti-platelet antibodies as well as the production of antibodies leading to apoptosis of megakaryocytes. We report the case of a gentleman who presented with evidence of acute inferior myocardial infarction in the setting of quinine-induced thrombocytopenia. We discuss the history and pathogenesis of quinine-induced thrombocytopenia as well as the relationship between platelet count and risk and outcome of myocardial infarction. The patient successfully underwent percutaneous coronary intervention and the placement of a bare metal stent, chosen in preference to a drug-eluting stent due to the wish to minimize the duration of dual anti-platelet therapy in the setting of thrombocytopenia. His platelets increased significantly with no intervention other than holding tonic water, and he suffered no bleeding complications related to catheterization. We conclude that cardiac catheterization can be successfully performed in the setting of quinine-induced thrombocytopenia and believe that this is one of the first reported cases of quinine-induced thrombocytopenia in the setting of myocardial infarction.
Keywords: Thrombocytopenia; Myocardial infarction
| Introduction | ▴Top |
The relationship between thrombocytopenia and the risk and outcome of myocardial infarction is not well defined. Quinine is a relatively rare cause of thrombocytopenia, likely mediated by quinine-induced production of anti-platelet antibodies as well as antibodies leading to apoptosis of megakaryocytes. We report the case of a gentleman who presented with inferior myocardial infarction in the setting of quinine-induced thrombocytopenia and underwent successful cardiac catheterization and stenting as well as demonstrate resolution of thrombocytopenia with withdrawal of quinine. Bare metal coronary stenting may be preferred to drug-eluting stent in this setting to minimize the duration of dual anticoagulant therapy with aspirin and clopidogrel.
| Case Report | ▴Top |
A 46-year-old male was transferred to this hospital for management of myocardial infarction and found to be thrombocytopenic. He had no known past medical history and had never seen a physician. He was in good health until 2 days prior to his presentation, when he developed dull, intermittent, non-radiating substernal chest pain at rest, not resolved with aspirin. He presented the following day to another hospital, where EKG (unavailable to us) reportedly demonstrated ST elevations. He was transferred to this hospital for further management; no medications were administered and no interventions were made prior to transfer.
Upon arrival to this hospital, the patient complained of substernal chest pain. Labs were notable for a platelet count of 20,000 with an otherwise normal CBC. Troponin was elevated at 1.14, and EKG demonstrated ST depression in leads V2-V3 without ST segment elevation. He was given aspirin (325 mg), clopidogrel (600 mg), and started on intravenous unfractionated heparin. Due to continued chest discomfort, eptifibatide was added. Platelet count the next morning remained low at 19,000 and hematology was consulted prior to cardiac catheterization.
At the time of hematologic evaluation, the patient was chest pain free. He had never had a blood test prior to this admission, and baseline platelet count was unknown. He endorsed occasional gum bleeding when brushing his teeth but denied any epistaxis, hematemesis, hemoptysis, hematuria, hematochezia, melena, petechiae, or purpura. He had no known family history of bleeding disorder. He was from Morocco and traveled between his home country and the United States fairly frequently. He denied any recent illness (febrile or otherwise). He did not take any medications, but did endorse drinking at least 1 L of tonic water daily for several months prior to presentation.
Physical exam was notable for lack of oral mucosal bleeding, petechiae, or purpura, cardiac exam with regular rate and rhythm and no murmurs or rub, clear lungs bilaterally, and lack of hepatosplenomegaly. Review of the peripheral smear demonstrated thrombocytopenia without platelet clumping or giant platelets. The differential diagnosis included idiopathic thrombocytopenic purpura (ITP), infection-related thrombocytopenia, or quinine-induced thrombocytopenia. Given the lack of giant platelets, ITP was thought to be unlikely. He had no history of recent viral prodrome, and though viral infection was possible, given his history, the leading suspicion was for quinine-induced thrombocytopenia.
Clinical outcome
The patient was observed for 4 days in the absence of tonic water. He was continued on aspirin, clopidogrel, and heparin. Troponin peaked at 2.43 and trended down thereafter. By day 4, platelet count had risen to 98,000. Cardiac catheterization performed at this time demonstrated tight ostial stenosis of the first diagonal of the left anterior descending artery, ostial occlusion of the second marginal branch of the left circumflex artery which filled via left to left collaterals, and an 80% mid right coronary artery (RCA) stenosis (Fig. 1). Left ventricular ejection fraction (LVEF) was 50% with mid-inferior and lateral wall hypokinesis. The RCA was dilated with a 2.5 mm balloon and an Integrity bare metal stent was placed with no residual stenosis in the area of the stent, and a 40% non-obstructive stenosis distal to the stent (Fig. 2). The patient tolerated the procedure well without evidence of bleeding. He was discharged on day 5 of his hospital stay in good condition with a platelet count of 105,000. Discharge medications included aspirin 81 mg daily, clopidigrel 75 mg daily, atorvastatin, lisinopril, and metoprolol succinate. To our knowledge, this is the first reported case of quinine-induced thrombocytopenia in the setting of acute myocardial infarction. Withdrawal of tonic water led to a rapid rise in platelet count and successful stent placement without bleeding complications.
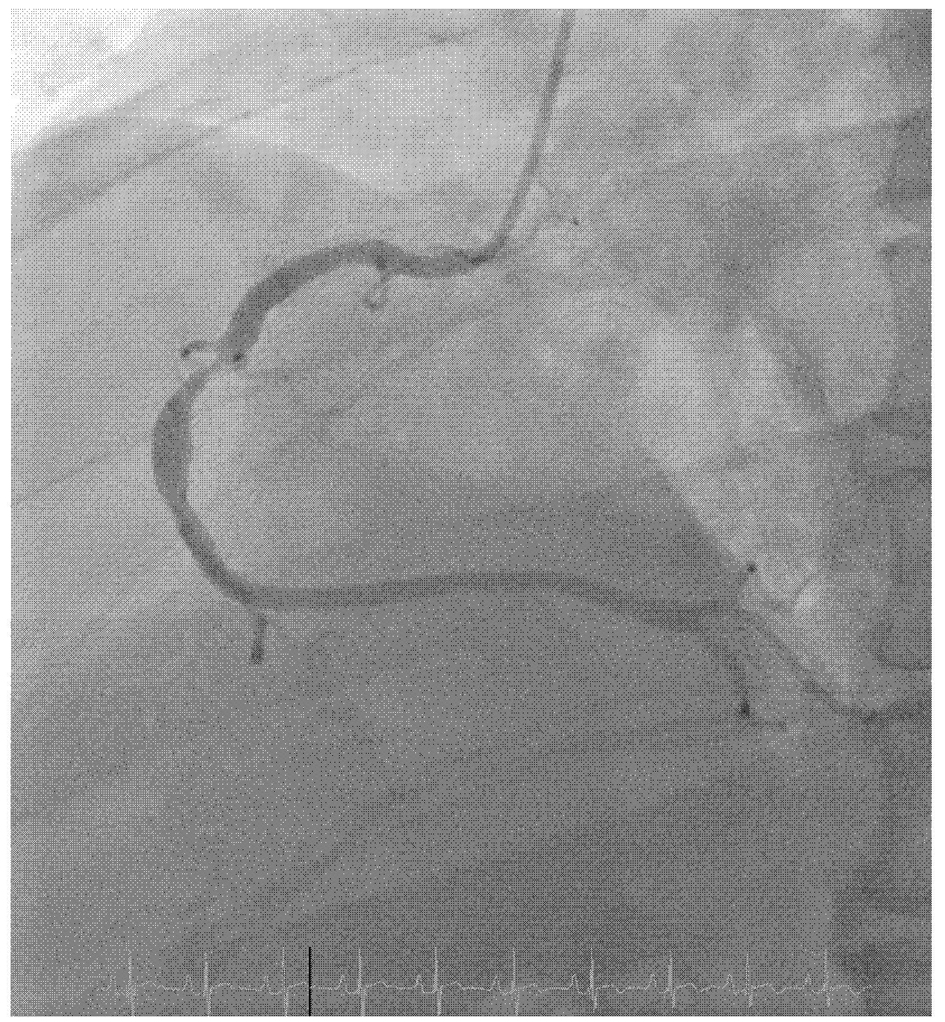 Click for large image | Figure 1. Cardiac catheterization performed demonstrated tight ostial stenosis of the first diagonal of the left anterior descending artery, ostial occlusion of the second marginal branch of the left circumflex artery which filled via left to left collaterals, and an 80% mid right coronary artery (RCA) stenosis. |
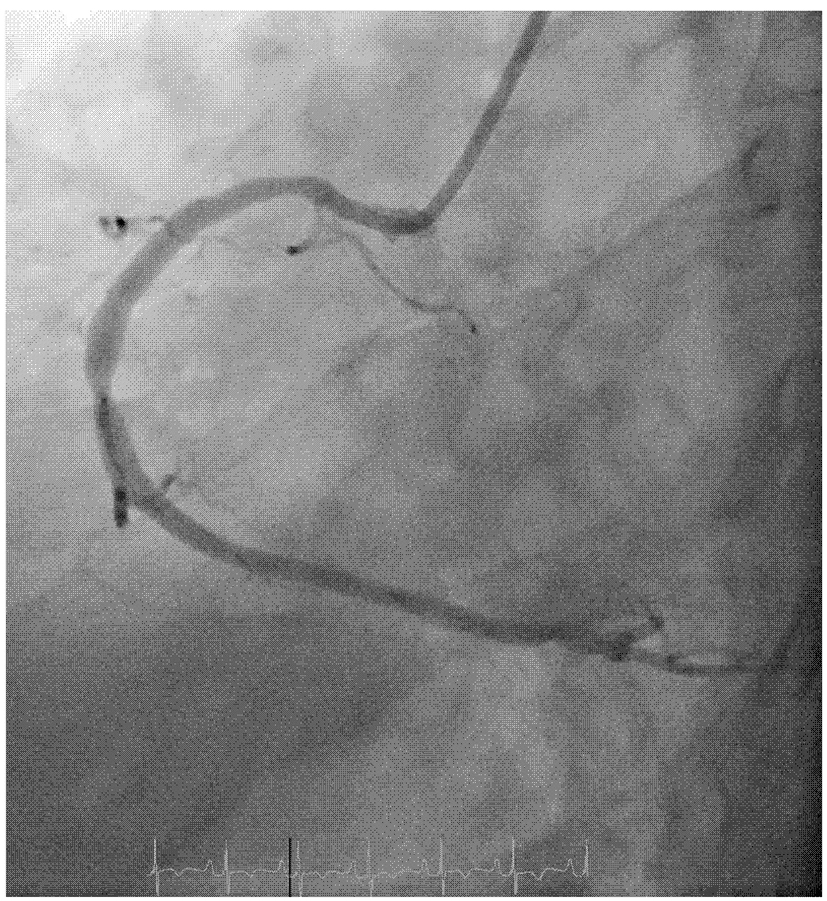 Click for large image | Figure 2. The RCA was dilated with a 2.5 mm balloon and an Integrity bare metal stent was placed with no residual stenosis in the area of the stent, and a 40% non-obstructive stenosis distal to the stent. |
| Discussion | ▴Top |
Quinine-induced thrombocytopenia
Quinine-induced bleeding was first reported in 1865, in a series of four cases where medical administration of quinine led to purpura, and in one case oral mucosal bleeding [1]. The dose of quinine required to lead to thrombocytopenia varies widely. One report of a man with cinchonism and purpura after drinking large quantities of gin and tonic estimated the patient’s intake at approximately 100 mg per day based on the Schweppes content of about 30 mg of quinine per pint. This patient’s symptoms resolved after 48 h of holding tonic and recurred with a test dose of 150 mg of quinine [2]. A large case series found that patients developed thrombocytopenic purpura at doses of quinine from 200 mg to over 10 g, and that time to development of symptoms varied widely but resolved quickly after cessation of quinine [3]. Current FDA regulations limit quinine in tonic water to 83 ppm or 83 mg/L [4], and it would not be impossible for a patient such as this taking in over 80 mg of quinine a day to develop thrombocytopenia.
The mechanism of quinine-induced thrombocytopenia is likely multifactorial. Anti-platelet antibodies may form in response to a drug-platelet complex, or quinine may bind to a plasma protein and induce anti-platelet antibody formation [5]. Additionally, IgG antibody produced in response to quinine has been shown to bind megakaryocytes, induce their apoptosis, and decrease proplatelet capacity in vitro [6].
Thrombocytopenia and myocardial infarction
The effect of thrombocytopenia on risk and outcome of myocardial infarction is not well defined. Elevated platelet count, such as seen in patients with essential thrombocythemia, is a risk factor for vascular thrombosis, likely through via platelet release of procoagulant microparticles and increase in thrombin generation [7]. Myocardial infarction has been reported in several patients with thrombocytosis and with essential thrombocythemia [8, 9]. However, myocardial infarction has also been reported in patients with idiopathic thrombocytopenia, and the authors propose a mechanism of antibody-mediated endothelial damage via autoantibodies directed against antigens present not only against platelets but also coronary endothelial cells [10]. This mechanism would likely be unique to patients with ITP rather than patients with thrombocytopenia induced in other situations.
Though there is certainly of an increased risk of bleeding, percutaneous coronary intervention (PCI) has been performed successfully in patients with thrombocytopenia (reported most often in the case of idiopathic thrombocytopenia); bare metal stents have generally been preferred to drug-eluting stents in order to limit the duration of dual anti-platelet therapy with aspirin and clopidogrel [11]. Use of aspirin and balloon angioplasty alone was complicated by restenosis in one case, requiring initiation of clopidogrel and stent placement [12].
The relationship between thrombocytopenia and clinical outcome is unclear. Thrombocytopenia has been associated with increased rates of bleeding, morbidity, and in-hospital mortality in patients who developed thrombocytopenia after the administration of anti-platelet or thrombolytic medications for acute myocardial infarction [13]. Baseline thrombocytopenia in patients undergoing angioplasty for ST-elevation myocardial infarction was an independent predictor for 30-day adverse events (bleeding, cardiac and non-cardiac events and death) but not 2-year events [14], and in this study platelet values were only reported at baseline and not over time and it is likely that thrombocytopenia had not resolved by the time of intervention as was the case with this patient.
Acknowledgement
We thank Dr. Kenneth Rosenfield, Section Head for Vascular Medicine and Intervention at Massachusetts General Hospital, for providing the images (Figs. 1 and 2) from the cardiac catheterization.
Financial Support and Disclosure
There were no specific sources of financial support for this case. The authors have no disclosures to report. This manuscript has not been presented at any meeting or published or presented in any other format.
| References | ▴Top |
- Vipan WH. Quinine as a cause of purpura. Lancet. 1865;2:37.
doi - Yohalem SB. Quinine in tonic water. JAMA. 1953;153:304.
doi - Bolton FG, Dameshek W. Thrombocytopenic purpura due to quinidine. I. Clinical studies. Blood. 1956;11(6):527-546.
pubmed - Quinine. http://www.gpo.gov/fdsys/pkg/CFR-2008-title21-vol3/pdf/CFR-2008-title21-vol3-sec172-575.pdf Accessed March 9, 2013.
- Shulman NR. Immunoreactions involving platelets. IV. Studies on the pathogenesis of thrombocytopenia in drug purpura using test doses of quinidine in sensitized individuals; their implications in idiopathic thrombocytopenic purpura. J Exp Med. 1958;107(5):711-729.
doi pubmed - Perdomo J, Yan F, Ahmadi Z, Jiang XM, Stocker R, Chong BH. Quinine-induced thrombocytopenia: drug-dependent GPIb/IX antibodies inhibit megakaryocyte and proplatelet production in vitro. Blood. 2011;117(22):5975-5986.
doi pubmed - Falanga A, Marchetti M. Thrombotic disease in the myeloproliferative neoplasms. Hematology Am Soc Hematol Educ Program. 2012;2012:571-581.
- Virmani R, Popovsky MA, Roberts WC. Thrombocytosis, coronary thrombosis and acute myocardial infarction. Am J Med. 1979;67(3):498-506.
doi - Nanavati A, Patel N, Burke J. Thrombocytosis and coronary occlusion. JACC Cardiovasc Interv. 2012;5(6):e18-19.
doi pubmed - Fruchter O, Blich M, Jacob G. Fatal acute myocardial infarction during severe thrombocytopenia in a patient with idiopathic thrombocytopenic purpura. Am J Med Sci. 2002;323(5):279-280.
doi pubmed - Gracia MC, Cebollero IC, Lezcano JS, Osuna GG, Miguel JA, Peralta LP. Invasive treatment performed for acute myocardial infarction in a patient with immune thrombocytopenic purpura. Int J Cardiol. 2008;127(3):e183-185.
doi pubmed - Stouffer GA, Hirmerova J, Moll S, Rubery B, Napoli M, Ohman EM, Simpson R. Percutaneous coronary intervention in a patient with immune thrombocytopenia purpura. Catheter Cardiovasc Interv. 2004;61(3):364-367.
doi pubmed - McClure MW, Berkowitz SD, Sparapani R, Tuttle R, Kleiman NS, Berdan LG, Lincoff AM, et al. Clinical significance of thrombocytopenia during a non-ST-elevation acute coronary syndrome. The platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrilin therapy (PURSUIT) trial experience. Circulation. 1999;99(22):2892-2900.
doi pubmed - Hakim DA, Dangas GD, Caixeta A, Nikolsky E, Lansky AJ, Moses JW, Claessen B, et al. Impact of baseline thrombocytopenia on the early and late outcomes after ST-elevation myocardial infarction treated with primary angioplasty: analysis from the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trial. Am Heart J. 2011;161(2):391-396.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


