| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 11, Number 2, April 2022, pages 62-65
Cyclical Thrombocytopenia Synchronized With the Patient’s Menstrual Cycle Treated With Danazol
Sasmith R. Menakurua, b, Adelina Priscua, Vijaypal Dhillona, Ahmed Saliha
aInternal Medicine, Indiana University Health, Ball Memorial Hospital, Muncie, IN 47303, USA
bCorresponding Author: Sasmith R. Menakuru, Internal Medicine, Indiana University Health, Ball Memorial Hospital, Muncie, IN 47303, USA
Manuscript submitted December 18, 2021, accepted February 7, 2022, published online March 12, 2022
Short title: CTP Synchronized With the Menstrual Cycle
doi: https://doi.org/10.14740/jh964
| Abstract | ▴Top |
Cyclical thrombocytopenia (CTP) is a very rare condition and often misdiagnosed as immune thrombocytopenia (ITP) due to similar features existing between the two. When evaluating a patient for the possible diagnosis of ITP, CTP must be high on the differential diagnosis. The main difference between the two conditions is that CTP is usually unresponsive to the treatment given to ITP and will ultimately display a cyclical nature with periods of low, normal and elevated platelets. As of date, there are only 70 cases in the literature. However, this number may be misrepresented due to the difficulty in diagnosis. The authors report a case of a 36-year-old woman who was misdiagnosed with ITP and underwent unnecessary treatment with corticosteroids, rituximab, intravenous immunoglobulins, and a splenectomy. A diagnosis of CTP was made after extensive review and the authors aim to bring awareness of this uncommon condition.
Keywords: Cyclical thrombocytopenia; Immune thrombocytopenia; Danazol
| Introduction | ▴Top |
Thrombocytopenia is defined as a platelet count below the lower limit of normal which is less than 150 × 103/µL for adults and can be divided into mild (100 - 150 × 103/µL), moderate (50 - 99 × 103/µL), and severe (< 50 × 103/µL) [1]. Thrombocytopenia can be associated with a variety of conditions including immune thrombocytopenia (ITP) and cyclical thrombocytopenia (CTP).
ITP is defined as isolated thrombocytopenia with a platelet count < 100 × 103/µL without anemia or leukopenia and without another apparent cause of thrombocytopenia [2]. CTP is characterized by periods of fluctuations in platelet counts, referring to the episodes of thrombocytopenia alternating with normal platelet counts with each cycle lasting 3 - 5 weeks [3]. Most cases are idiopathic without an underlying hematological condition. However, some patients may rarely display CTP in myeloproliferative and myelodysplastic syndromes. Patients with the idiopathic form, such as in our patient, are often misdiagnosed as having ITP and are treated as such, despite poor response [4]. Physicians may attribute the rise in platelet counts to treatment. However, the disease itself is cyclical in nature. If physicians consider CTP as a diagnosis, then a period of observation is indicated with graphing of platelet counts to check for fall, rebound and if platelet nadirs occur during menstrual periods for females [4]. Treatment of the condition is case based but there are reports that danazol, cyclosporin A, and medroxyprogesterone acetate have worked for patients. However, the long-term course of CTP is obscure with some cases achieving complete remission but with others rebounding [5].
| Case Report | ▴Top |
Investigations
A 36-year-old female presented to the outpatient clinic as a new patient with a history of symptomatic thrombocytopenia causing mucosal bleeding and easy bruising. She recently moved across the country for a new job opportunity. She stated she was diagnosed with ITP as her platelet counts were low and otherwise healthy with no other medical conditions of note. She said that she had heavy menstrual bleeding and that she would use between 9 and 11 pads per day. She also noticed her gums were bleeding while brushing her teeth and, occasionally, she would bruise easily. In one instance, she said that she was expecting a bruise because she fell but that she did not develop any bruising. She had no other episodes of bleeding and denied hematuria, hematemesis, and hematochezia. She had no family history of blood disorders or any history of cancer.
Laboratory investigations revealed platelet counts of 9 × 103/µL, hemoglobin 9.8 g/dL, hematocrit 31%, mean corpuscular volume 76 fL, mean corpuscular hemoglobin 32 g/dL, mean corpuscular hemoglobin concentration 33.9 g/dL, and ferritin 101 mg/L.
Platelet-bound and free anti-glycoprotein (GP) IIb/IIIa and anti-GPIb/IX autoantibodies were found to be negative from samples taken from peripheral blood using the standard direct and indirect antigen capture assays, respectively. Hepatitis and human immunodeficiency virus (HIV) panels were negative. Peripheral blood smear showed hypochromic, microcytosis, and normal platelet and leukocyte morphology. There were no abnormal cells present on the peripheral smear as well. She started taking oral iron for her iron deficiency anemia.
As the patient was previously diagnosed with ITP and was very proactive about keeping her medical records, she had a complete list of all her laboratory results and treatment plans. All other potential etiologies of isolated thrombocytopenia were ruled out including rheumatological conditions, malignancy, drug-induced ITP, hepatitis C and liver disease, HIV, herbal remedies, familiar conditions including hereditary thrombocytopenia, thyroid disease, pseudo thrombocytopenia, and myelodysplastic syndrome. An extensive chart review was done, which found that the patient’s platelet counts would decrease to lows of around 10 × 103/µL but in a few instances the platelet levels were around 400 × 103/µL. The patient was first treated with pulse oral dexamethasone 40 mg for 4 days. On initiation of dexamethasone her platelet count was 9.4 × 103/µL, and on the follow-up visit her count was 8 × 103/µL. She was then given pulse dexamethasone for two more cycles. During the initiation of her third cycle, she was found to have a platelet count of 90 × 103/µL but then was found to have a count of 12 × 103/µL at the end of the 4 days. She was then deemed to have failed glucocorticoids and was therefore started on rituximab as she wanted to avoid a splenectomy. She was put on rituximab 375 mg/m2 intravenously for 4 weeks, where she had platelet counts of 11 × 103/µL, 230 × 103/µL, 130 × 103/µL, and 15 × 103/µL. She was then put on eltrombopag 50 mg orally for 2 weeks which did not raise platelet counts as well as she was found to have a platelet count of 17 × 103/µL at the end of treatment. She was told that since her platelet counts were not improving, a splenectomy would be the next best choice for treatment. Even though she initially opposed surgery, she agreed. Unfortunately, she did not have an adequate response to the splenectomy as platelet counts did not stabilize and would fall 10 - 50 × 103/µL in most platelet counts. A bone marrow biopsy was done to check for myelodysplastic syndrome. However, it was negative. Afterward, she was put back on rituximab of which she had two doses before transitioning care.
Diagnosis
As suspicion was high for CTP as a differential diagnosis for ITP given the chart review, she was told to come to the clinic weekly for 3 months to check platelet counts and that rituximab would not be continued (Fig. 1). The cyclical nature of her platelet count was established with lows corresponding to her menstrual period and she was therefore diagnosed as having CTP.
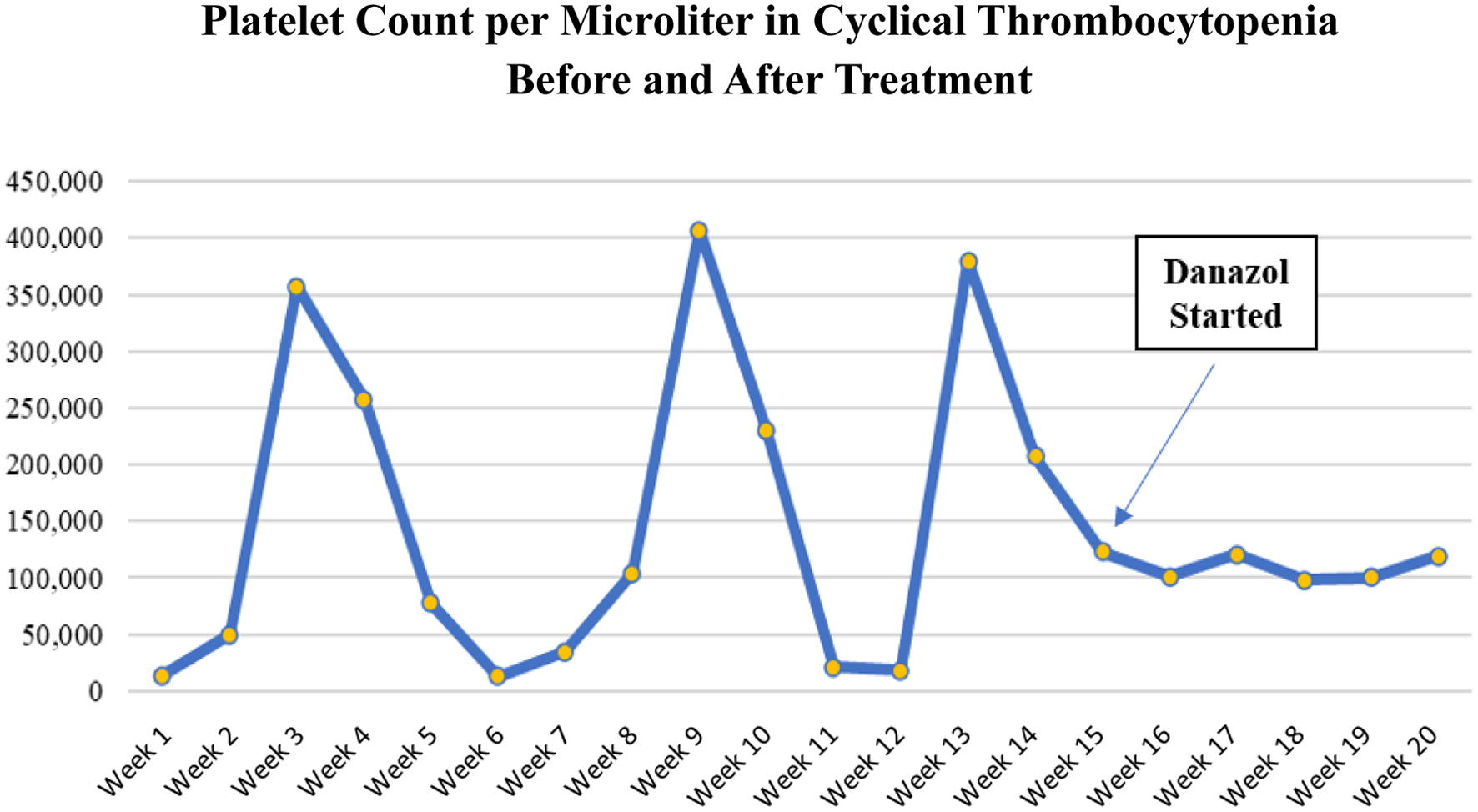 Click for large image | Figure 1. Platelet counts per microliter in cyclical thrombocytopenia before and after treatment with danazol. Platelet nadirs correlate to the patient’s menstrual cycle and a cyclical nature is clearly demonstrated. Danazol was started on the 14th week (as shown by arrow) and stabilized platelet counts around 100 × 103/µL. |
Treatment
Treatment was started with danazol due to its reduction in estrogen production and levels, and that has been proven effective in CTP by multiple other case reports.
Follow-up and outcomes
During her 6 months of follow-up, she did not report any episodes of major bleeding. Her menstrual flow has improved, not requiring as many pads daily and she said that she was not bruising as easily anymore. On danazol, her platelet counts stabilized around 100 × 103/µL. She will continue to follow up with the outpatient clinic.
| Discussion | ▴Top |
CTP is a rare disorder characterized by the cyclic oscillation of platelet counts, with distinct phases of thrombocytopenia and thrombocytosis causing platelet counts to become normal or elevated. CTP is more often found in females, with a median age of 35 years [4]. During the phase of thrombocytopenia bleeding either mild or severe can occur, which is the presenting symptom for most patients. Due to the low platelet counts, many individuals are diagnosed as having ITP, therefore patients are treated with glucocorticoids and immunoglobulins which are first-line treatments for it. However, after inevitable treatment failure patients may be subjected to either splenectomy, rituximab, or thrombopoietin receptor antagonists, such as in our patient.
The reason for misdiagnosis is often due to the transient rise of platelets being attributed to treatment. However, there will ultimately be a relapse with a low platelet count which is then attributed to treatment failure. The cyclical nature of the disease and lack of knowledge about the disorder is the root cause of delayed diagnosis as the interval between the diagnosis of ITP to the final diagnosis of CTP is usually many years [6]. This is in part because of the similar nature of the two disorders, as both CTP and ITP usually present in healthy young women with menorrhagia, as well as the absence of organomegaly and lymphadenopathy [7]. In a review done by Go, it was found that out of 51 cases of CTP published at that time, almost all the cases did not have CTP in the differential diagnosis of ITP [4]. An early diagnosis would prevent patients from undergoing harmful unnecessary therapies.
The pathogenesis of the condition is unknown. There are some leading theories, including autoimmune platelet destruction, a clonal T cell-mediated process, megakaryocytic hypoplasia, and defects in the processes that regulate platelet formation [7]. Many patients with CTP exhibit the presence of antiplatelet antibodies with an inverse relationship to platelet count, and there is also an inverse relationship between platelet counts and levels of thrombopoietin [6]. In an observational study done by Steinbrecher et al, a relationship between CTP and disorders of the thyroid gland and hematological malignancy was suggested, but no clear association was mentioned. In the study, the largest of its kind on CTP, all the eight women had underlying thyroid disease [5]. The diagnosis of CTP can be made in patients with a high degree of suspicion for the disorder by utilizing frequent blood count monitoring without treatment which will demonstrate the cyclical nature of thrombocytopenia [6]. As CTP presents more frequently in women, there is also a close relation to thrombocytopenia during periods of menses [8]. In our case, platelets cycled in synchrony with her menstrual cycle which helped solidify the diagnosis. Even though CTP is most often seen in young premenopausal females, it may also present in men and postmenopausal women [9]. The cycles of thrombocytopenia and thrombocytosis usually occur every 3 - 4 weeks. Long-term follow-up of patients with CTP may be required as there are reports that patients may develop hematological or thyroid disorders [6].
The treatment of CTP is based on case reports and observational studies. There are no set treatment protocols. Some patients do not require treatment as spontaneous remission may occur. However, in those that do, cyclosporin A and hormone therapy, such as progestin or danazol, can be used. The relationship between female hormone levels and platelet cycling is the reason why danazol was chosen in our case. The response to treatment is varied as some achieve stable platelet counts and some patients achieve remission. Therefore, response to the treatment is individually based. More research must be done about the pathogenesis and treatment of the disease as this would increase the identification, provide better forms of treatment, and would provide better outcomes of patients suffering from CTP [10].
Conclusions
Physicians should be aware of CTP as a cause of thrombocytopenia, and therefore it must be part of the differential diagnosis in any patient presenting with ITP refractory to treatment. Demonstration of the cyclical course of the disease can be done by repeated follow-up and tracking platelet counts without treatment. In women, a relationship may be made between low levels of platelets and menstrual periods, which would support the diagnosis of CTP. The authors believe this case is important in current literature as it details the many failed treatment options that the patient had to go through before the diagnosis of idiopathic CTP was made, which brings to light the need for an early diagnosis as it can help patients avoid the unnecessary treatment of ITP.
Learning points
CTP is a rare disorder characterized by fluctuating platelet counts every 3 - 4 weeks resulting in thrombocytopenia with subsequent rebound thrombocytosis to elevated or normal counts. The prevalence of CTP may be hindered by a diagnosis of ITP but should be looked for in young women with platelet nadirs occurring during their menstrual period along with graphing platelet counts demonstrating the cyclical nature of the disease. CTP should be high on the differential diagnosis of any patient with treatment-resistant ITP as an early diagnosis of CTP would allow for better outcomes. Patients who are suspected of having CTP should be monitored every week over several weeks to see if a cyclical cycle of platelets is present. Long-term monitoring of patients with CTP is necessary as patients are known to develop hematological and thyroid disorders. Patients can be treated with cyclosporin A or danazol, but close monitoring and follow-up are required as there is a lack of response in most.
Acknowledgments
No acknowledgments to declare.
Financial Disclosure
No funding to declare.
Conflict of Interest
No conflict of interest to declare.
Informed Consent
Informed consent was taken from the patient, and she fully agreed with the text written.
Author Contributions
SRM saw the case, did research, and wrote the case report. AP helped with research, writing, and editing. VD and AS helped with editing.
Data Availability
The authors declare that data supporting the findings of the study are available within the article.
| References | ▴Top |
- Williamson DR, Albert M, Heels-Ansdell D, Arnold DM, Lauzier F, Zarychanski R, Crowther M, et al. Thrombocytopenia in critically ill patients receiving thromboprophylaxis: frequency, risk factors, and outcomes. Chest. 2013;144(4):1207-1215.
doi pubmed - Rodeghiero F, Stasi R, Gernsheimer T, Michel M, Provan D, Arnold DM, Bussel JB, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009;113(11):2386-2393.
doi pubmed - Minot GS. Purpura hemorrhagica with lymphocytosis: an acute type and an intermittent menstrual type. Am J Med Sci. 1936;192:445-456.
doi - Go RS. Idiopathic cyclic thrombocytopenia. Blood Rev. 2005;19(1):53-59.
doi pubmed - Steinbrecher O, Mitrovic M, Eischer L, Sinkovec H, Eichinger S, Kyrle PA. Clinical and laboratory characteristics of cyclic thrombocytopenia: an observational study. Haematologica. 2020;105(4):e198-e201.
doi pubmed - Kyrle PA, Eichinger S. How I manage cyclic thrombocytopenia. Blood. 2021;137(2):178-184.
doi pubmed - Dogara LG, Sani A, Waziri AD, Taingson MC, Mohammed AS. Cyclic thrombocytopenia associated with menorrhagia. Trop J Obstet Gynaecol [serial online]. 2016;33:337-339.
doi - Haurie C, Dale DC, Mackey MC. Cyclical neutropenia and other periodic hematological disorders: a review of mechanisms and mathematical models. Blood. 1998;92(8):2629-2640.
doi pubmed - Menitove JE, Pereira J, Hoffman R, Anderson T, Fried W, Aster RH. Cyclic thrombocytopenia of apparent autoimmune etiology. Blood. 1989;73(6):1561-1569.
doi pubmed - Samanani S, Khanna S, Mujahid R, Asik A. Cyclical Thrombocytopenia - a rare but fatal imitator of idiopathic thrombocytopenia. Blood. 2017;130(Supplement 1):4860. ISSN 0006-4971.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


