| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 12, Number 5, October 2023, pages 231-235
Cyclic Thrombocytopenia in the Setting of Intracranial Hemorrhage: A Diagnostic and Therapeutic Challenge
Ryan Sweeneya, d, Maitreyee Raib, Harmeet Kharoudc, Rama Bhagavatulab, Robert Kaplanb, Deep Shahb
aDepartment of Internal Medicine, Allegheny Health Network, Pittsburgh, PA, USA
bDivision of Hematology and Cellular Therapy, Allegheny Health Network Cancer Institute, Allegheny Health Network, Pittsburgh, PA, USA
cDepartment of Pathology, Allegheny Health Network, Pittsburgh, PA, USA
dCorresponding Author: Ryan Sweeney, Department of Internal Medicine, Allegheny Health Network, Pittsburgh, PA 15212, USA
Manuscript submitted July 16, 2023, accepted September 22, 2023, published online October 21, 2023
Short title: CTP and Cerebral Bleeding
doi: https://doi.org/10.14740/jh1171
| Abstract | ▴Top |
Cyclic thrombocytopenia (CTP) as the name suggests presents with cyclic episodes of thrombocytopenia and is frequently initially misdiagnosed as immune thrombocytopenia. Following a lack of sustained response or abnormally increased response to common treatments used for immune thrombocytopenia, a proper diagnosis of CTP can then be made. Prior reports have shown a subset of patients who respond to cyclosporin A. Here, we present a case of CTP that was initially at another facility presumed to have and treated for immune thrombocytopenic purpura. However, after multiple attempts to treat with steroids, intravenous immunoglobulin (IVIG), rituximab, and eltrombopag, episodes of severe thrombocytopenia followed by thrombocytosis continued. The patient ultimately developed intracerebral hemorrhage (ICH) in the setting of one of the episodes of severe thrombocytopenia and developed multiple subsequent complications from which the patient unfortunately did not recover. It was only after developing ICH that the patient had been evaluated at a center with hematology consultation capabilities, at which time after a detailed review of his case and pattern recognition the proper diagnosis of CTP was made with initiation of cyclosporine. This case was further complicated by need to maintain an adequate platelet threshold post-ventriculoperitoneal shunt placement which was necessary due to his ICH and was placed before diagnosis of CTP could be made. While CTP is a rare diagnosis, this case reinforces a greater need to properly diagnose and consider cyclosporine treatment for CTP, as it has been effective in some patients and may help to prevent patient morbidity and especially catastrophic bleeding complications.
Keywords: Thrombocytopenia; Intracranial hemorrhage; Cerebral intraventricular hemorrhage; Cyclosporine
| Introduction | ▴Top |
Cyclic thrombocytopenia (CTP) is a rare platelet disorder characterized by periodic, predictable, episodes of severe thrombocytopenia that occur every 3 - 5 weeks [1]. Patients with CTP are often misdiagnosed with immune thrombocytopenia (ITP) and only after thrombocytopenia fails to improve with standard ITP therapies is the correct diagnosis often identified [2]. Treatment of CTP is challenging with limited options that have been shown to be effective. For a subset of CTP patients, cyclosporine A has been shown to be an effective treatment method [3-5]. Here, we report the case of a patient who was diagnosed with CTP after frequent admissions with thrombocytopenia that was unresponsive to common ITP therapies and presented with intracranial hemorrhage, for whom treatment required maintaining a platelet threshold of > 5.0 × 104/µL in the setting of neurosurgical interventions.
| Case Report | ▴Top |
Investigations
A 70-year-old male with history of immune thrombocytopenia (presumed), gastric bypass surgery complicated by iron deficiency anemia and vitamin B12 deficiency, diabetes mellitus, chronic kidney disease, obstructive sleep apnea, pulmonary fibrosis, and aqueductal stenosis with cerebral ventriculomegaly who recently underwent right endoscopic third ventriculostomy presented with altered mental status. Patient was at an inpatient rehab facility where he was found to be confused and unable to respond to questioning 9 days after third ventriculostomy procedure. He was also noted to have prominent tremulousness of his extremities. Computed tomography (CT) of head revealed acute intracerebral and third ventricular hemorrhage. CT angiogram of the head and neck demonstrated moderate- to high-grade multifocal narrowing. He was intubated for airway protection and was admitted to the neuro-intensive care unit for further evaluation and management.
Initial laboratory workup was notable for severe thrombocytopenia with platelet count of 1.4 × 104/µL, white blood cell count of 8.84 × 103/µL, hemoglobin of 11.4 g/dL, erythrocyte sedimentation rate of 18 mm/h, and C-reactive protein of < 0.4 mg/dL. Patient responded well to platelet transfusion and maintained platelet count > 1.00 × 105/µL. He underwent emergent external ventricular drain placement followed by right frontal ventriculoperitoneal shunt placement without complication. Hematology was consulted for recommendations regarding management of thrombocytopenia.
Looking back on his prior history, we noted that the patient had multiple recurrent admissions at an outside hospital for severe thrombocytopenia over the course of the preceding year with platelet counts as low as 3 × 103/µL (Fig. 1). Patient underwent extensive prior workup during his initial admission for his thrombocytopenia including lactate dehydrogenase, haptoglobin, fibrinogen, fibrin degradation products, international normalized ratio (INR), vitamin B12, folate, and serum copper which were all within normal limits. Infectious workup including human immunodeficiency virus (HIV), hepatitis C, Epstein-Barr virus, and cytomegalovirus serologies were negative and an autoimmune workup including rheumatoid factor, antinuclear antibody, antiphospholipid antibody syndrome panel, and serum protein electrophoresis were unremarkable. He was diagnosed with presumed immune thrombocytopenic purpura (ITP) and was treated with dexamethasone and intravenous immunoglobulin (IVIG) with rapid platelet improvement initially to 7.5 × 104/µL a few days after discharge. However, patient continued to develop recurrent episodes of thrombocytopenia necessitating several hospitalizations for steroids and IVIG. Ultimately, he was initiated on rituximab with initial improvement in thrombocytopenia, but again developed severe thrombocytopenia with nadir of 4 × 103/µL. A bone marrow biopsy was performed and revealed normocellular marrow with trilineage hematopoiesis and slightly decreased megakaryocytes (Fig. 2). Flow cytometry on the bone marrow was unremarkable. Platelet count on the date of bone marrow biopsy was 3.1 × 104/µL. The patient was ultimately started on eltrombopag with reactive thrombocytosis to 1.324 × 106/µL. Eltrombopag was thus intermittently held with large fluctuations in platelet counts on and off the medication, reaching > 1.000 × 106/µL on multiple occasions (even at doses as low as 25 mg every other day) but paradoxically with recurrence of thrombocytopenia thereafter.
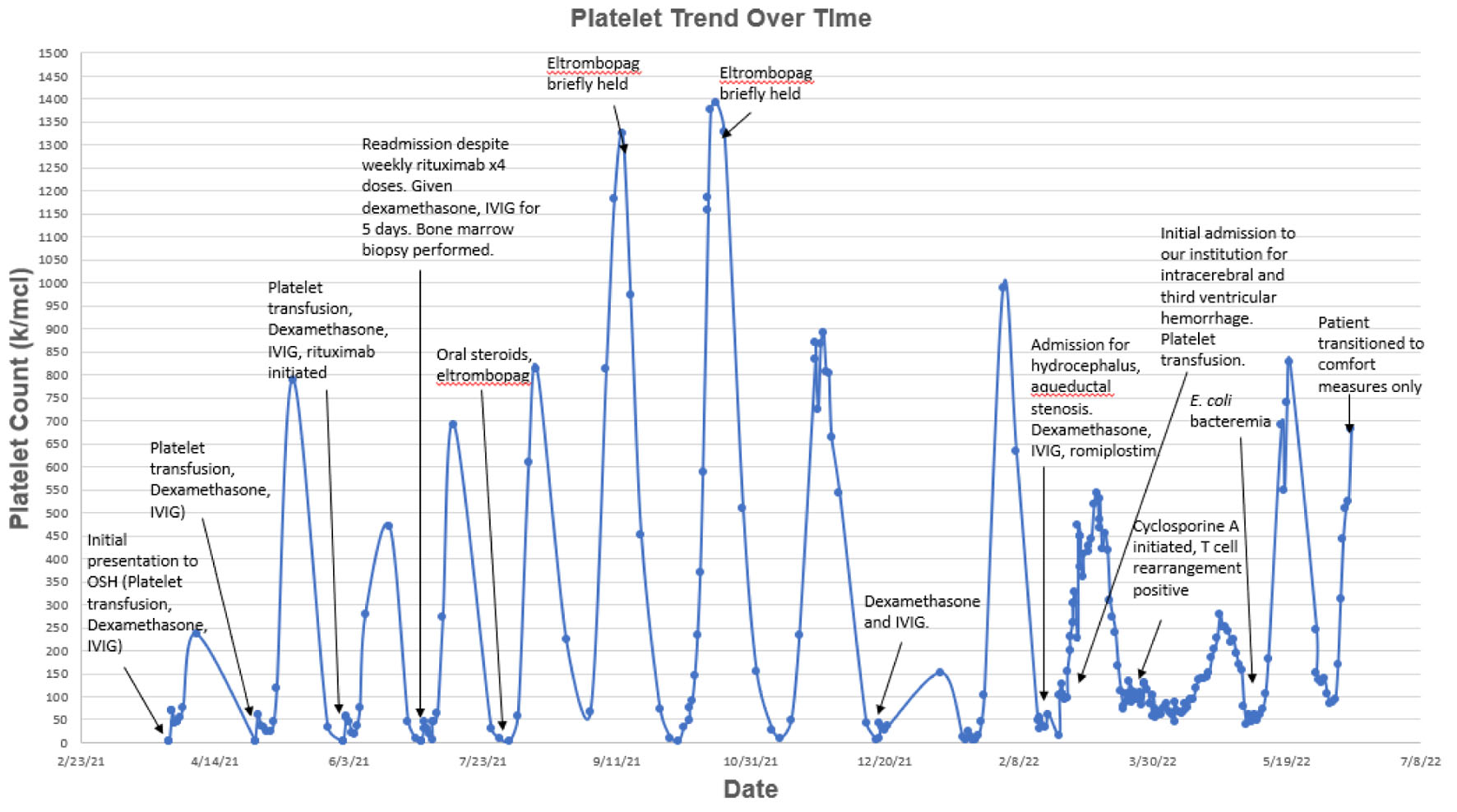 Click for large image | Figure 1. Platelet count over time. Patient presented to our institution with intracerebral and third ventricular hemorrhage at which time hematology was consulted. Looking back on prior platelet trends, patient had been hospitalized multiple times for recurrent episodes of severe thrombocytopenia. Upon pattern recognition, a diagnosis of cyclic thrombocytopenia was made and patient was initiated on cyclosporine A. Platelets stabilized to > 5.0 × 104/µL, a threshold recommended by neurosurgery in the setting of ventriculoperitoneal shunt placement, for nearly 3 months. |
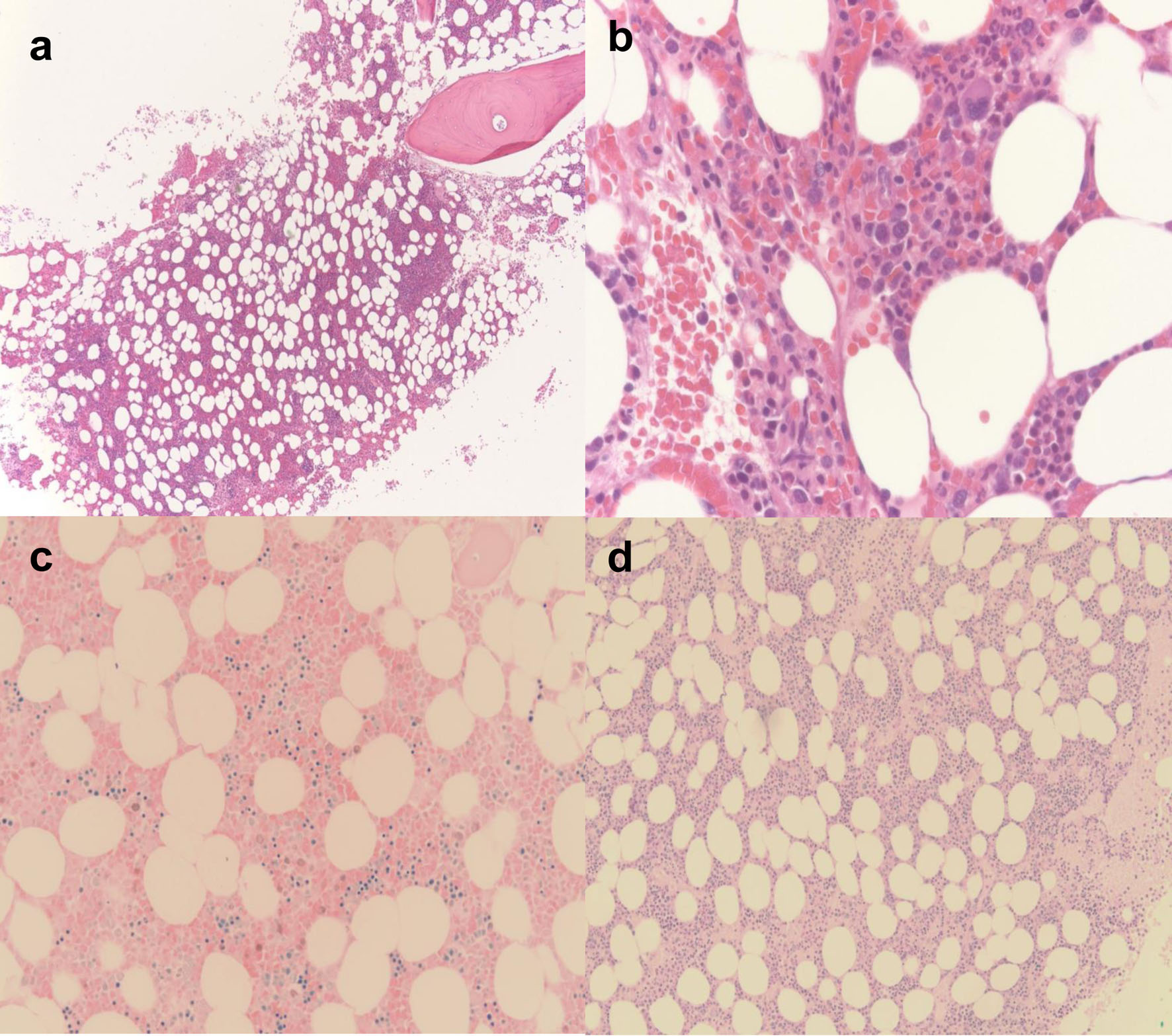 Click for large image | Figure 2. Bone marrow biopsy findings. (a) Low power × 2 magnification: the cellularity is 30%. Megakaryocytes are slightly decreased with minimal atypia. The myeloid to erythroid ratio appears unremarkable. (b) High power × 20: single megakaryocyte is visible with minimal atypia. (c) Giemsa stain: it shows normal myeloid to erythroid ratio. (d) Periodic acid-Schiff (PAS) stain: it shows normal myeloid to erythroid ratio. |
Diagnosis
We noted on review of his medical chart that the patient was refractory to all the above treatments for ITP while also having unusually high response to eltrombopag. Hence, we began to challenge the diagnosis. After reviewing platelet trends over the prior year, it was apparent that the patient would reach a nadir in his platelet counts every 25 - 30 days regardless of ITP treatment. Given the cyclic fluctuations in his platelet counts, lack of sustained response to treatment or inexplicable platelet count in relation to treatment, and decreased megakaryocytes on prior bone marrow biopsy, there was clinical concern for CTP. Additionally, patient was found to have a positive clonal T-cell beta change rearrangement (TRB D+J1/2).
Treatment
Patient was initiated on cyclosporine post-operatively with initial stabilization of platelet count and discharge to inpatient rehab. In order to maintain a platelet count > 5.0 × 104/µL (as recommended by neurosurgery to prevent ICH in setting of ventriculoperitoneal shunt placement), eltrombopag was restarted and ultimately titrated to dosing every 48 h to prevent rebound thrombocytosis while maintaining a platelet count of at least 50,000.
Follow-up and outcomes
A few weeks after initiating cyclosporine, platelets dropped to nadir of 4.4 × 104/µL for 1 day and improved rapidly with transfusion. Otherwise, platelets remained stably > 5.0 × 104/µL for the remaining 3 months of the patient’s life aside from one brief drop in platelets to nadir of 3.9 × 104/µL in the setting of E. coli and E. cloacae bacteremia after which platelets responded quickly to transfusion and treatment of the underlying infection. Unfortunately, further medical complications mounted, including aspiration pneumonia, bacteremia, and pneumoperitoneum after which his family elected to pursue comfort measures only and the patient subsequently died.
| Discussion | ▴Top |
CTP is a rare disorder presenting with periodic fluctuations of platelet counts, often with a nadir as low as < 5 × 103/µL fluctuating with normal platelet counts or rebound thrombocytosis, with or without treatment. Platelet fluctuations occur predictably, with thrombocytopenia episodes occurring every 3 - 5 weeks [1]. CTP is exceedingly rare, representing in one study less than 1% of all cases of ITP [2]. It predominantly affects females and can coexist with thyroid disorders [2, 6]. When seen in females, platelet trend can follow the menstrual cycle, with platelet nadir occurring at the onset of menses [3]. Patients often are misdiagnosed with ITP and a diagnosis of CTP is made after failure to develop sustained platelet response to common ITP therapies along with excessive response to thrombopoietin (TPO) agonists when platelet counts peak in the cycle, as seen in our patient who was treated multiple times with steroids, IVIG, rituximab, and eltrombopag [2, 7].
The pathogenesis of CTP remains unclear. In a few case reports, patients with CTP have been found to have a clonal T-cell receptor rearrangement suggesting that this could be a T-cell-mediated disease [3, 8, 9]. In one study, a patient found to have CTP went on to develop T-cell large granular lymphocytic leukemia [8]. However, additional potential mechanisms could also contribute. Subsets of patients with CTP have been found to have auto-antibodies, and thrombopoietin levels have been shown to have an indirect correlation with platelet count, suggesting potential contribution from autoimmune platelet destruction and impaired thrombopoiesis [8]. Additionally, given the predilection towards females and correlation of thrombocytopenia with the menstrual cycle, there may be a hormonal contribution to pathogenesis. Similar to ITP, patients with CTP are more likely to have an underlying thyroid disorder [8, 10, 11]. Our patient was a male without any underlying thyroid disorder or autoimmune disorder; however, he was found to have a positive T-cell receptor rearrangement with cyclical platelet counts irrespective of active treatment, suggestive of CTP.
Treatment of CTP remains challenging, with limited therapies shown to prevent cyclic platelet fluctuations. Traditional management for ITP, including corticosteroids, IVIG, rituximab, romiplostim, and eltrombopag, is typically ineffective in preventing the severe drops in platelet counts that are intrinsic to the disease process [1, 8, 9, 12]. Platelet transfusions must be given prudently, given the risk of alloimmunization and the possibility for emergent need to transfuse platelets in the setting of active bleeding, as seen in our patient who developed acute intracerebral and third ventricular hemorrhage. Treatment with cyclosporine A has shown reported benefit to a subset of patients with CTP [3-5]. However, the predictors of response are unknown [13].
In our patient, after remaining on cyclosporine for at least 1 month, platelet counts remained stable in the 1.50 × 105/µL - 2.50 × 105/µL range with the exception of one episode of thrombocytopenia to 3.9 × 104/µL in the setting of E. coli and E. cloacae bacteremia. It should be noted that platelet count stabilization was also accomplished by eltrombopag, which was initiated out of need to maintain platelets at least > 5.0 × 104/µL given recent ventriculoperitoneal shunt placement (placed due to presenting ICH), which provided an additional complicating factor in management of this case. Unfortunately, our patient would go on to develop multiple complications from which he ultimately died. Thus, it is unclear what the long-term efficacy of cyclosporine A would have been in our patient; however, an improvement in platelet cycling was initially demonstrated. Aside from a brief drop in platelets thought to be secondary to bacteremia, platelets remained at the 5.0 × 104/µL threshold recommended by neurosurgery for nearly 3 months after initiation of cyclosporine A until the patient’s death from unrelated causes, including gastric ulcer perforation and tension pneumoperitoneum.
Given the severe, recurrent episodes of thrombocytopenia that characterize this disorder, it is imperative to identify and properly treat the correct diagnosis early in order to prevent patient morbidity and use of unnecessary ITP-related therapy. There remains a possibility that if diagnosis had been made sooner and appropriate treatment with cyclosporine initiated sooner, the severe thrombocytopenia that facilitated ICH and the subsequent cascade complications and hospitalizations that likely hastened the patient’s death may have been ultimately preventable. Thus, increasing provider awareness through such case reports remains necessary.
Learning points
CTP presents with cyclical episodes of thrombocytopenia. It is often misdiagnosed as immune thrombocytopenia and often fails to provide a lack of sustained response or abnormally increased response to common treatments for immune thrombocytopenia. A subset of patients has been shown to respond to cyclosporine A, as was seen in our patient. Prompt diagnosis and initiation of appropriate treatment is imperative in order to prevent bleeding complications due to severe, recurrent thrombocytopenia.
Acknowledgments
The authors have no acknowledgments.
Financial Disclosure
The authors have no sources of funding to disclose.
Conflict of Interest
The authors have no conflict of interest to disclose.
Informed Consent
Not applicable as no patient-identifying information is present in manuscript.
Author Contributions
All authors participated in the construction of the manuscript. RS, MR, RB, RK, and DS all participated in treating the patient. HK provided the bone marrow biopsy images.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Go RS. Idiopathic cyclic thrombocytopenia. Blood Rev. 2005;19(1):53-59.
doi pubmed - Arnold DM, Nazy I, Clare R, Jaffer AM, Aubie B, Li N, Kelton JG. Misdiagnosis of primary immune thrombocytopenia and frequency of bleeding: lessons from the McMaster ITP Registry. Blood Adv. 2017;1(25):2414-2420.
doi pubmed pmc - Tomer A, Schreiber AD, McMillan R, Cines DB, Burstein SA, Thiessen AR, Harker LA. Menstrual cyclic thrombocytopenia. Br J Haematol. 1989;71(4):519-524.
doi pubmed - Kyrle PA, Eichinger S. How I manage cyclic thrombocytopenia. Blood. 2021;137(2):178-184.
doi pubmed - Steinbrecher O, Mitrovic M, Eischer L, Sinkovec H, Eichinger S, Kyrle PA. Clinical and laboratory characteristics of cyclic thrombocytopenia: an observational study. Haematologica. 2020;105(4):e198-e201.
doi pubmed pmc - Fogarty PF, Stetler-Stevenson M, Pereira A, Dunbar CE. Large granular lymphocytic proliferation-associated cyclic thrombocytopenia. Am J Hematol. 2005;79(4):334-336.
doi pubmed - Fureder W, Mitterbauer G, Thalhammer R, Geissler K, Panzer S, Krebs M, Simonitsch-Klupp I, et al. Clonal T cell-mediated cyclic thrombocytopenia. Br J Haematol. 2002;119(4):1059-1061.
doi pubmed - Chen G, Chen L, Qin X, Xie X, Li G, Xu B. Cyclic thrombocytopenia related to menstrual cycle: a case report and literature review. Int J Clin Exp Med. 2014;7(10):3595-3598.
pubmed pmc - Cheung E, Liebman HA. Thyroid disease in patients with immune thrombocytopenia. Hematol Oncol Clin North Am. 2009;23(6):1251-1260.
doi pubmed - Bose P, Hussein KK, Terrell DR, Berger D, Rice L, George JN. Successful treatment of cyclic thrombocytopenia with thrombopoietin-mimetic agents: a report of two patients. Am J Hematol. 2009;84(7):459-461.
doi pubmed - Zent CS, Ratajczak J, Ratajczak MZ, Anastasi J, Hoffman PC, Gewirtz AM. Relationship between megakaryocyte mass and serum thrombopoietin levels as revealed by a case of cyclic amegakaryocytic thrombocytopenic purpura. Br J Haematol. 1999;105(2):452-458.
pubmed - Telek B, Kiss A, Pecze K, Ujhelyi P, Rak K. Cyclic idiopathic pure acquired amegakaryocytic thrombocytopenic purpura: a patient treated with cyclosporin A. Br J Haematol. 1989;73(1):128-129.
doi pubmed - Rice L, Nichol JL, McMillan R, Roskos LK, Bacile M. Cyclic immune thrombocytopenia responsive to thrombopoietic growth factor therapy. Am J Hematol. 2001;68(3):210-214.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


