| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 13, Number 4, August 2024, pages 164-167
Optic Disc Infiltration as a Sign of Multiple Myeloma Recurrence
Maria Pantelidoua, Eleni Dimitrioua, Konstantinos Gkontopoulosb, Thomas Thomopoulosb, Vasiliki Pappab, Sotirios G. Papageorgioub, Panagiotis Theodossiadisa, Irini Chatzirallia, c
a2nd Department of Ophthalmology, Attikon University Hospital, National and Kapodistrian University of Athens, Athens, Greece
b2nd Department of Propaedeutic Internal Medicine, Hematology Unit, Attikon University Hospital, National and Kapodistrian University of Athens, Athens, Greece
cCorresponding Author: Irini Chatziralli, 2nd Department of Ophthalmology, Attikon University Hospital, National and Kapodistrian University of Athens, Athens, Greece
Manuscript submitted March 19, 2024, accepted August 5, 2024, published online August 15, 2024
Short title: Optic Disc Infiltration in Multiple Myeloma
doi: https://doi.org/10.14740/jh1267
| Abstract | ▴Top |
Multiple myeloma is a plasma cell dyscrasia with an age-standardized incidence of 3 - 4 per 100,000 in the Caucasian population. It is the second most common hematological malignancy after non-Hodgkin lymphoma, representing 1% of all cancers. Herein, we present a case report of multiple myeloma with ocular involvement as a sign of recurrence. A 62-year-old woman, with a known history of lambda light chain multiple myeloma, presented with reduced visual acuity in both eyes while on maintenance chemotherapy. The patient also had mild unsteadiness and fatigue. Fundus examination revealed bilateral optic disc swelling and hemorrhages of the posterior pole. Magnetic resonance imaging disclosed no abnormalities. Although no biopsy of the optic nerve was possible, intracranial pressure was elevated and cerebrospinal fluid was riddled with neoplastic cells, affirming the diagnosis. After 2 months of chemotherapy, visual function and the appearance of the posterior pole returned to normal. In cases of multiple myeloma, mechanisms, such as hyperviscosity syndrome, microvascular impairment and optic nerve and meningeal infiltration on a cellular level may have played a pivotal role in the ocular involvement, which can be the first sign of recurrence.
Keywords: Optic disc infiltration; Multiple myeloma; Recurrence; Ocular involvement
| Introduction | ▴Top |
Multiple myeloma is a plasma cell dyscrasia with an age-standardized incidence of 3 - 4 cases per 100,000 in the Caucasian population, making it the second most common hematological malignancy after non-Hodgkin lymphoma and representing 1% of all cancers [1, 2]. The median age of occurrence appears to be between 56 and 66 years [3, 4].
Ocular manifestations of multiple myeloma include depositions of myelomatous, calcium or amyloid crystals in the anterior chamber, salmon conjunctival patch, eyelid ecchymosis, necrotizing xanthogranuloma, light chain deposits in the cornea, iris or ciliary epithelium cysts, anterior and/or posterior uveitis, retinal hemorrhages, venous congestion, cotton wool spots, optic nerve infiltration, disc swelling and orbital plasmacytoma possibly compromising eye movement [5, 6]. Despite its variety, ocular involvement is rare, although it may be present at the diagnosis [7], scarcely as the first sign of the disease [8-11], or may occur after several months of onset [7]. It has also been described as the first symptom of recurrence, while on maintenance therapy [12]. Herein, we report a case of optic nerve infiltration, as a sign of recurrence in a patient with multiple myeloma.
| Case Report | ▴Top |
A 62-year-old woman was referred to our ophthalmology department with a 5-day bilateral painless decrease in vision, transient diplopia, weakness and mild unsteadiness. The patient’s ocular history included no ophthalmic conditions except for mild myopia, which has been so far corrected by eyeglasses. Regarding her medical history, a diagnosis of lambda (λ) light chain multiple myeloma was established 2 years ago, after a pathological O1 fracture. She had then undergone six sessions of radiotherapy on the fracture site and six cycles of treatment with bortezomib (Velcade), lenalidomide (Revlimid) and dexamethasone. After 1 year of maintenance of bortezomib plus dexamethasone, she had autologous stem-cell transplantation and for the past year, she was on maintenance chemotherapy with only lenalidomide.
At the initial ophthalmologic examination, best-corrected visual acuity (BCVA) was 0.4 logMAR in the right eye and 0.22 logMAR in the left eye. There was no relative afferent pupillary defect (RAPD) in both eyes. Color perception was tested normal (21/21 on Ishihara test) in both eyes. Confrontation visual field examination showed no defect in both eyes. Eye movements were full, the eyes were aligned and the initially referred diplopia at the horizontal eye position was not present when re-evaluated. Slit-lamp examination was normal regarding the anterior chamber. There were no signs of inflammation or infection. The intraocular pressure (IOP) was normal bilaterally (14 mm Hg).
Dilated fundoscopy revealed optic disc swelling and flame-shaped retinal hemorrhages in both eyes, much more severe in the right eye, while several dot-blot hemorrhages were present at the posterior pole accompanied by a pre-retinal hemorrhage in the right eye (Fig. 1). Optical coherence tomography (OCT) was performed, showing no macular edema in the right eye and a small serous retinal detachment at the foveal area in the left eye (Fig. 2a, b).
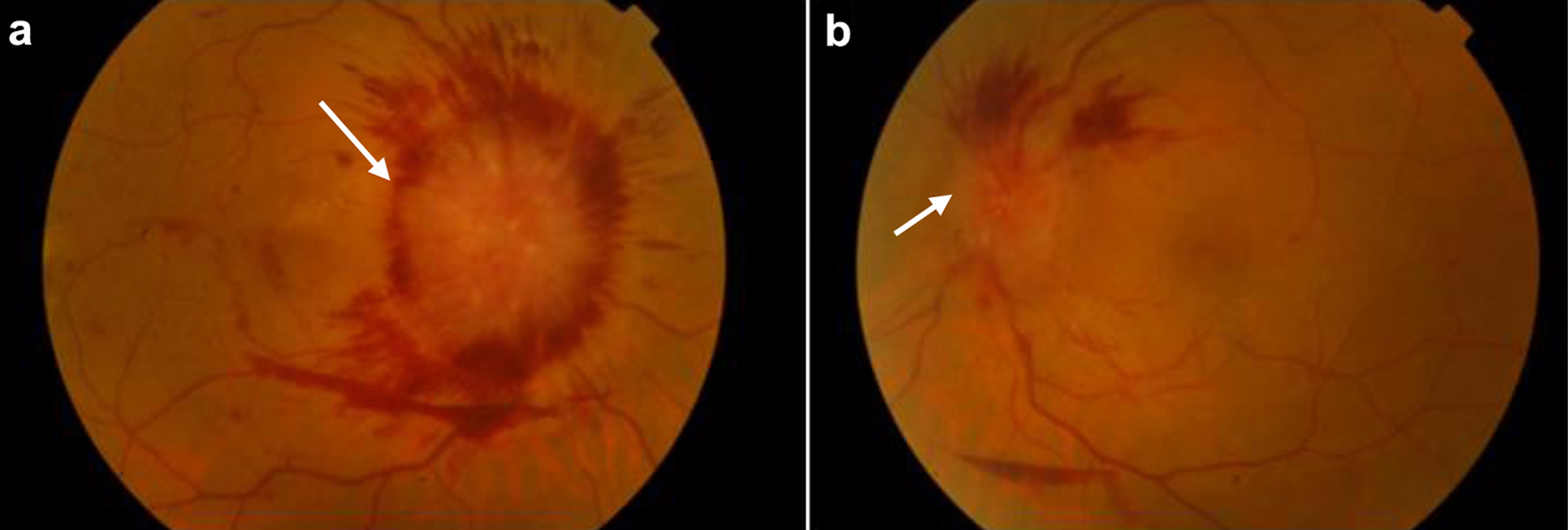 Click for large image | Figure 1. (a) Color fundus photograph of the right eye, showing extensive optic disc swelling (white arrow) with flame-shaped retinal hemorrhages around the optic disc, as well as dot-blot hemorrhages at the foveal area and a pre-retinal hemorrhage inferior of the optic disc. (b) Color fundus photography of the left eye, showing optic disc swelling (white arrow) and flame-shaped retinal hemorrhages superior to the optic disc, as well as a small pre-retinal hemorrhage adjacent to the inferior arcade. |
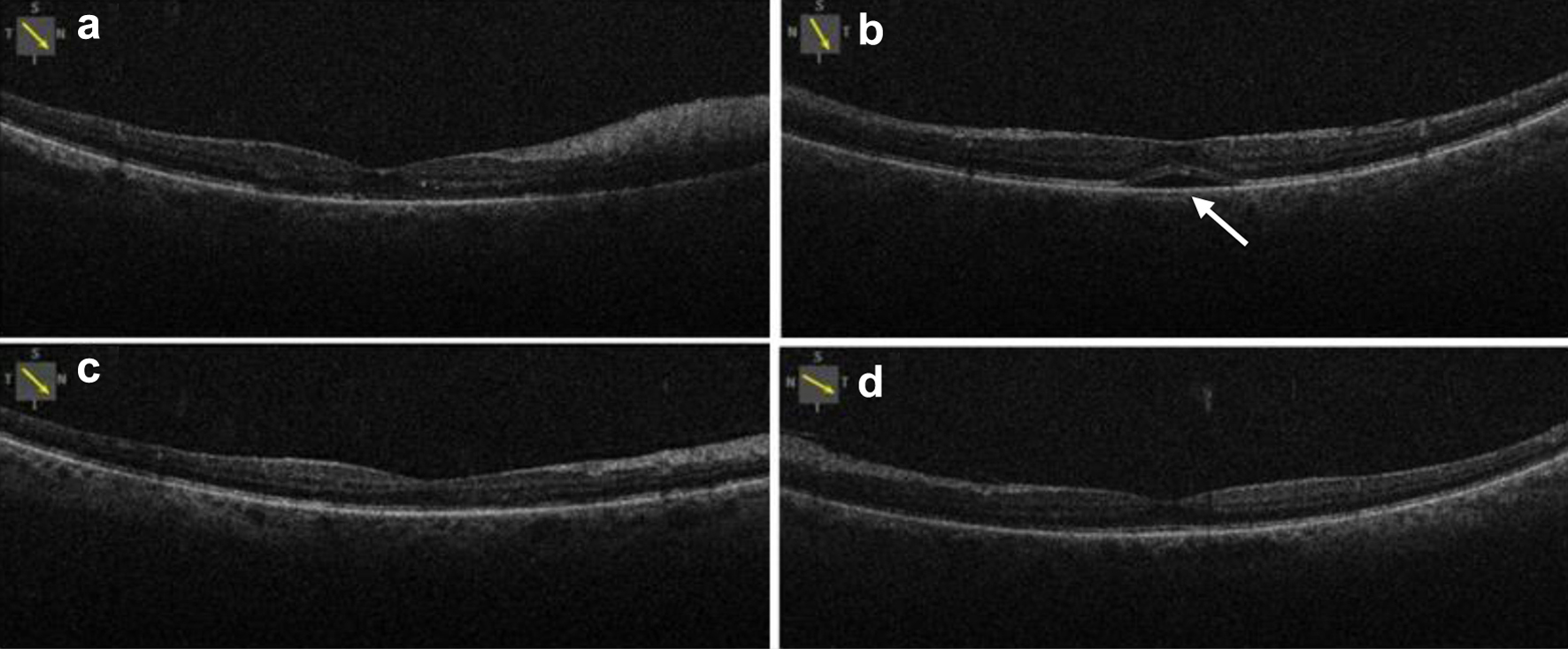 Click for large image | Figure 2. Optical coherence tomography of the right (a) and left (b) eye, showing normal macula in the right eye and small serous retinal detachment (white arrow) in the left eye at baseline. Optical coherence tomography of the right eye (c) and left (d) eye, showing normal retinal in both eyes with absorption of fluid in the left eye. |
Magnetic resonance imaging (MRI) was performed but demonstrated no signs of malignant disease. Lumbar puncture revealed an elevation of intracranial pressure at 33 mm Hg, so cerebrospinal fluid (CSF) drainage was performed as the first step to papilledema’s resolution. Additionally, CSF analysis proved the presence of many malignant plasma cells.
Hence, diagnosis of multiple myeloma recurrence was established and a new loading phase of treatment with bortezomib, lenalidomide and dexamethasone was started.
Fifteen days after initiation of treatment, BCVA improved to 0.22 logMAR in the right eye and to 0.16 logMAR in the left eye. Fundoscopy showed improvement, but there was still optic disc swelling and flame-shaped retinal hemorrhages in both eyes. After 2 months of treatment adherence, BCVA elevated to 0.09 logMAR in both eyes and fundoscopy revealed important alterations with almost full absorption of hemorrhages bilaterally, except for the pre-retinal one in the right eye (Fig. 3). There was a partial regression of disc swelling in the right eye, while almost resolved in the left eye. New OCT scan was normal in both eyes, with a total resolution of fluid in the left eye (Fig. 2c, d).
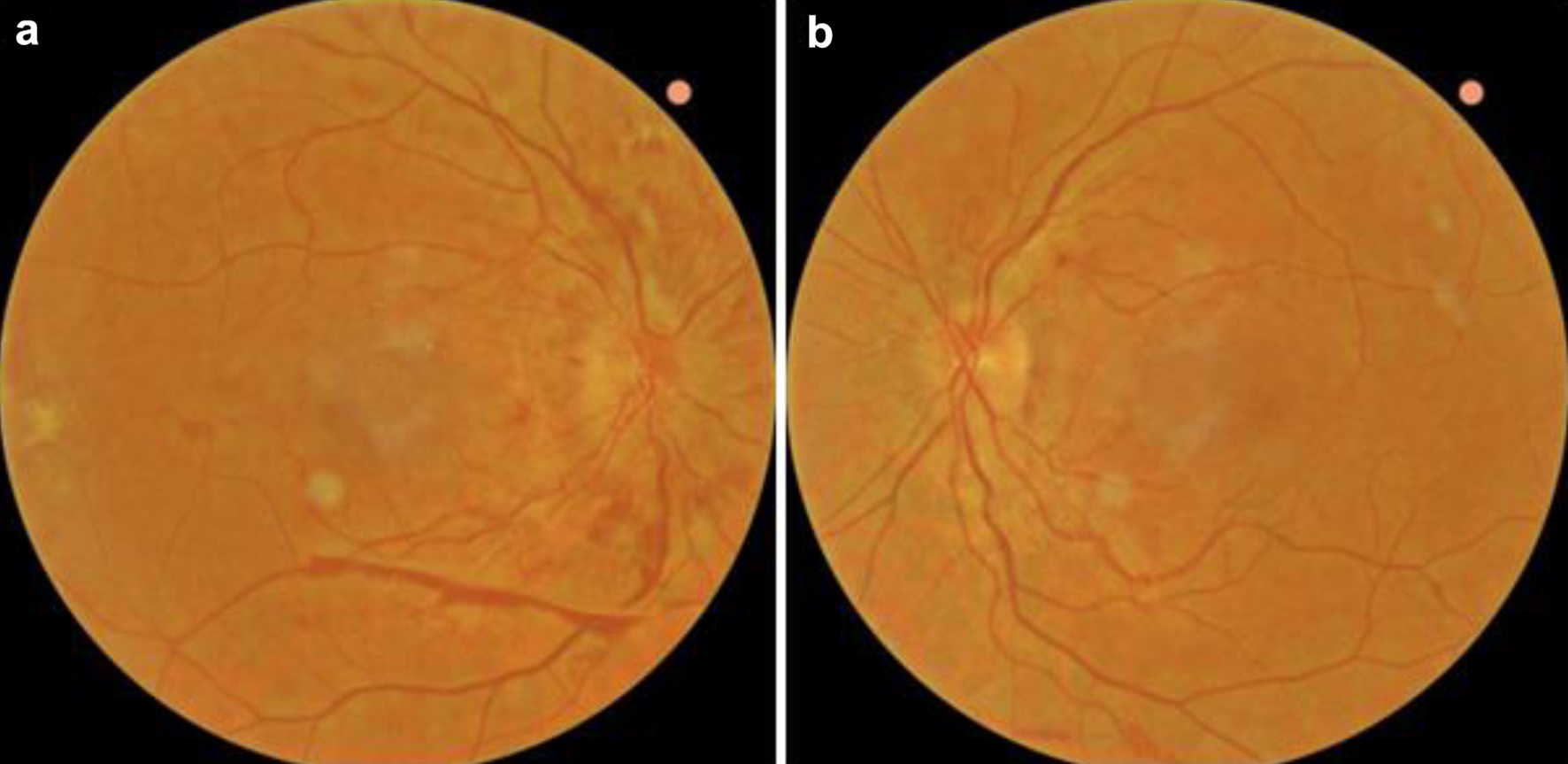 Click for large image | Figure 3. Color fundus photographs of the right (a) and left (b) eye 2 months after initiation of chemotherapy, showing improvement of the optic disc swelling in both eyes and almost full regression of retinal hemorrhages. |
| Discussion | ▴Top |
Our case stands up for a rare chance of orbital involvement in lambda light chain multiple myeloma, whereas the existing literature supports that heavy chain (mostly IgG and IgA) multiple myeloma is more likely to have ocular manifestations [7]. It becomes explicit that a multiple myeloma recurrence might occur with the ocular symptoms to be prevalent and hopefully very well responding to optimal therapy. Thus, recognition of the ocular signs and immediate initiation of treatment are crucial for the outcome.
Regarding the potential mechanisms of ocular damage, several pathways have been described. Retinal hemorrhages in our case are probably a result of hyperviscosity syndrome [13], as our patient’s platelet rate and coagulation factors were tested normal in every examination. An impairment of vascular supply due to aggregated intraluminal neoplastic cells and hypergammaglobulinemia [8] might be a substantial component of the case. The elevated ICP contributes partially to the optic disc swelling, but we strongly assume neoplastic infiltration at a cellular level as well. That is in accordance with the absence of a detectable lesion in the MRI and to the rapid positive response to chemotherapy, whereas CSF drainage had a minor effect on the regression. A possible meningeal infiltration of neoplastic cells may explain the neurological symptoms of fatigue and unsteadiness as well, which may be compatible with the elevated ICP, but withdrawn only after chemotherapy. Additionally, high levels of immunoglobulin have been documented to lead to a humoral mechanism that results in peripheral neuropathy [14]. Thus, there is a hypothesis that excessive immunoglobulin compromises neural conduction in the optic nerve, leading to painless vision loss. However, this deduction applies more to IgG multiple myeloma [9, 14].
The good visual outcome of our patient owes its presence to the absence of any fibrous subretinal tissue or degenerative damages in the retinal pigment epithelium, as it was demonstrated on OCT, that could preclude visual improvement, as mentioned in other case studies [10]. The short duration of the papilledema was also a main target of the treatment, so that visual decrease would only be transient.
In conclusion, our case study reveals that multiple myeloma recurrence might occur with dominant ocular manifestations, even while on maintenance therapy, and it may sufficiently be suppressed via the right time of intervention. Variability of the signs and the mimic character of the disease should be taken into account, so as to offer the optimal monitoring to these patients.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they do not have any conflict of interest.
Informed Consent
Written informed consent was obtained from the patient.
Author Contributions
MP and IC drafted the manuscript. All authors were involved in the diagnosis, treatment and follow-up of the patient, critically revised the manuscript, read, and approved the current version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Kazandjian D. Multiple myeloma epidemiology and survival: A unique malignancy. Semin Oncol. 2016;43(6):676-681.
doi pubmed pmc - Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57(1):43-66.
doi pubmed - Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, Fonseca R, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21-33.
doi pubmed - Levin SR, Spaulding AG, Wirman JA. Multiple myeloma. Orbital involvement in a youth. Arch Ophthalmol. 1977;95(4):642-644.
doi pubmed - Riccardi A, Gobbi PG, Ucci G, Bertoloni D, Luoni R, Rutigliano L, Ascari E. Changing clinical presentation of multiple myeloma. Eur J Cancer. 1991;27(11):1401-1405.
doi pubmed - Singh RB, Singhal S, Sinha S, Cho J, Nguyen AX, Dhingra LS, Kaur S, et al. Ocular complications of plasma cell dyscrasias. Eur J Ophthalmol. 2023;33(5):1786-1800.
doi pubmed pmc - Fung S, Selva D, Leibovitch I, Hsuan J, Crompton J. Ophthalmic manifestations of multiple myeloma. Ophthalmologica. 2005;219(1):43-48.
doi pubmed - Burkat CN, Van Buren JJ, Lucarelli MJ. Characteristics of orbital multiple myeloma: a case report and literature review. Surv Ophthalmol. 2009;54(6):697-704.
doi pubmed - Yeung SN, Paton KE, Dorovini-Zis K, Chew JB, White VA. Histopathologic features of multiple myeloma involving the optic nerves. J Neuroophthalmol. 2008;28(1):12-16.
doi pubmed - Shimada Y, Shibuya M, Ohki R, Yoneya S, Nakamura Y. Bilateral optic neuropathy associated with multiple myeloma. J Neuroophthalmol. 2006;26(2):117-120.
doi pubmed - Yilmaz SG, Ture G, Zengin MO, Talay E, Men S. Optic nerve and dura mater involvement as the first sign of multiple myeloma. Eur J Ophthalmol. 2015;25(1):77-79.
doi pubmed - Rao K, Murthy H, Muralidhar NS, Rani PK. Multiple myeloma masquerading as diabetic macular oedema. BMJ Case Rep. 2018;2018:bcr-2017-223485.
doi pubmed pmc - Nugent AK, Paulus YM, Chan A, Kim JW, Schwartz EJ, Moshfeghi DM. Multiple myeloma recurrence with optic nerve infiltration diagnosed by vitrectomy, immunohistochemistry, and in situ hybridization. Eur J Ophthalmol. 2014;24(3):446-448.
doi pubmed - Cox JG, Steiger MJ, Pearce JM. Optic neuropathy and multiple myeloma. Br J Hosp Med. 1988;39(5):448.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


