| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 3, Number 2, June 2014, pages 43-45
Treatment for Factor V Leiden, Stuck Between a Rock and a Hard Place: A Case Report and Review of Literature
Waqas Jehangira, c, Souad Enakuaaa, Victoria Udezib, Nilma Malika, Shuvendu Sena, Abdalla Yousifa, Mohammed A Islama
aRaritan Bay Medical Center, Perth Amboy, NJ 08861, USA
bRoss University School of Medicine, USA
cCorresponding Author: Waqas Jehangir, Raritan Bay Medical Center, Perth Amboy, NJ 08861, USA
Manuscript accepted for publication May 9, 2014
Short title: Treatment for Factor V Leiden
doi: https://doi.org/10.14740/jh149w
| Abstract | ▴Top |
Factor V Leiden is a genetically inherited disorder which causes hypercoagulable state that accounts for 40-50% of cases of thrombophilia. The diagnosis of factor V Leiden thrombophilia is made either by using a coagulation screening test or by DNA analysis of F5, which encodes the factor V protein. Management of this disorder can be challenging due to the fact that the current treatment regimen can place the patient in a bleeding state with potential hazardous effects. We are reporting the case of a 49-year-old man who presented with shortness of breath diagnosed with multiple episodes of pulmonary embolisms, DVT and factor V Leiden deficiency treated with oral anticoagulants again presented with dizziness and upper GI bleed.
Keywords: Factor V Leiden; Pulmonary embolism; Thrombophilia
| Introduction | ▴Top |
Factor V Leiden thrombophilia is named after the city Leiden in the Netherlands. Factor V Leiden is an autosomal dominant genetic disorder with incomplete dominance in which a mutation in the F5 gene causes thrombophilia (Fig. 1). There is a G-to-A substitution in the factor V gene leading to an amino acid replacement in one of the three APC cleavage sites in the factor Va molecule [1]. Due to this point mutation, factor V cannot be inactivated by activated protein C, hence there is an increased tendency to form abnormal blood clots that can block blood vessels.
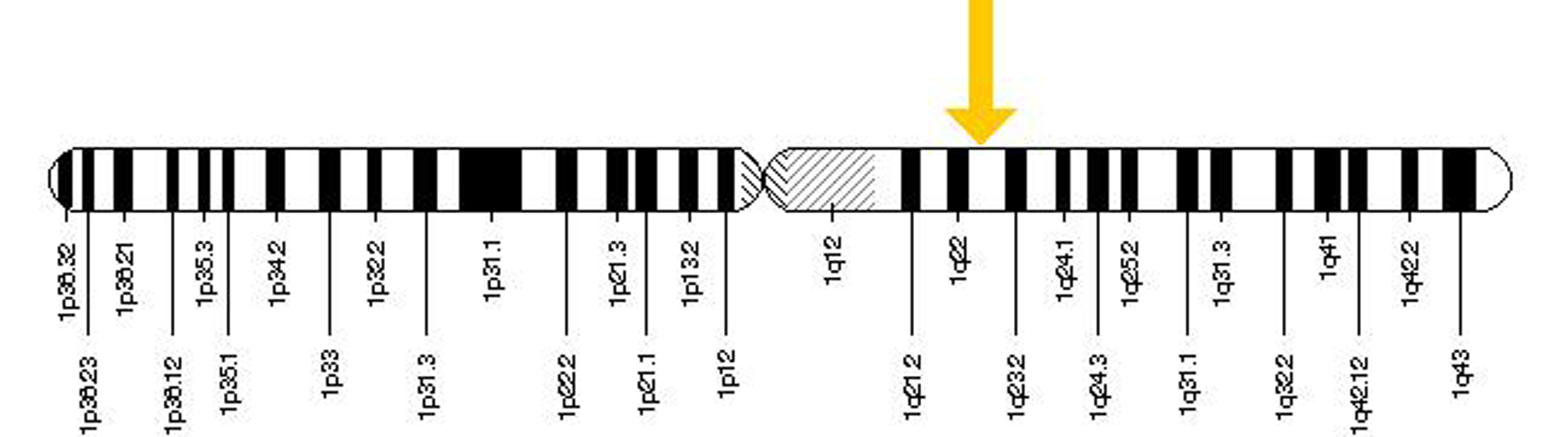 Click for large image | Figure 1. The F5 gene is located on the long (q) arm of chromosome 1 at position 23. |
Venous thromboembolism affects about 1 of every 130 persons younger than 65 years of age [2]. Factor V Leiden is the most common cause of inherited thrombophilia accounting for 40-50% of cases [1]. People with factor V Leiden thrombophilia have a higher-than-average risk of developing venous thromboembolic disease. The relative risk for venous thrombosis is increased approximately three to eightfold in individuals who are heterozygous for the factor V Leiden allele. It increased 18 to 80 fold in individuals who are homozygous [3]. This can manifest as DVTs, pulmonary embolisms or other venous outflow obstructions.
Factor V Leiden thrombophilia is diagnosed either by using a coagulation screening test or by DNA analysis of F5, which encodes the factor V protein [3]. Managing this disorder is challenging, because the current treatment regimen available can increase the patient’s chance of bleeding.
We are reporting the case of a 49-year-old man who was diagnosed with pulmonary embolism, DVT and factor V Leiden deficiency who later presented with dizziness and upper GI bleed.
| Case Report | ▴Top |
A 49-year-old male without any significant past medical history presented to the ED with worsening shortness of breath for 4 days which was gradual in onset, accompanied by a dry cough associated with right sided moderate pleuritic chest pain that was intermittent, alleviated by rest and aggravated by coughing. Patient also had an unintentional 30 lbs weight loss within the last month. He has 120 packs per year smoking history. Patient denied any recent travel or sick contact. He was not taking any medications and did not have any allergies.
On physical exam, the patient was tachycardic and tachypnic with mild respiratory distress and had decreased breath sounds on the right side. The rest of the exam was unremarkable. Laboratory data revealed hemoglobin of 7.5 g/dL, WBC of 11.9 and platelets 347,000. CXR showed a large right sided pleural effusion and right upper lobe opacity. CT scan of the chest showed multiple pulmonary emboli and patient had an extensive right lower extremity DVT on venous Doppler. Patient was started on heparin drip and then Coumadin. Vasculitis work-up was negative. Six weeks later, hypercoagulable work-up revealed factor V Leiden mutation (heterozygous).
Patient was advised to continue Coumadin and follow-up INR regularly upon discharge. Patient then presented twice within one year with similar symptoms of dizziness, loss of consciousness and melena. Patient was diagnosed with upper GI bleeding and coagulopathy secondary to anticoagulants. EGD was performed which showed multiple linear ulcerative lesion in the body of stomach without active bleeding. Anticoagulants were stopped briefly and he was treated with vitamin K, PRBC and fresh frozen plasma transfusion.
This patient had first been given Coumadin subsequently Rivaroxaban and then switched back to Coumadin after recurrent GI bleed. After 6 months of treatment patient stopped taking medication and later developed another DVT. Later, he was counseled that he needs life-long anticoagulation as he had recurrent DVT. He was restarted on Coumadin with close monitoring of INR in the clinic.
| Discussion | ▴Top |
There remains a need for adequate management to create a therapeutic balance in which the patient avoids a hypercoagulable state and does not end up in bleeding state due to the anticoagulation therapy.
Current management of factor V Leiden is based on the clinical manifestations in the patient. In the absence of a history of thrombosis, long-term prophylactic anticoagulation is not routinely recommended for asymptomatic factor V Leiden heterozygotes [3]. Patients should be counseled about eliminating certain risk factors like smoking and educated on the signs and symptoms of a DVT or PE so that early diagnosis and treatment may be instituted.
When risk factors are present, a short course of prophylactic anticoagulation may prevent initial thrombosis. In addition, patients may require temporary treatment with an anticoagulant during periods of particularly high risk, such as major surgery [4]. For patients with confirmed deep vein thrombosis or pulmonary embolism, anticoagulant therapy with subcutaneous low molecular-weight heparin, monitored IV, or subcutaneous unfractionated heparin or fondaparinux can be used [5].
As in our patient, an initial course of intravenous unfractionated heparin or low molecular-weight heparin can be started followed by initiation of warfarin except when contraindicated [4]. In our case, the patient has the heterozygous factor V Leiden mutation but with pulmonary embolism and DVT needed anticoagulation.
Long-term management of patients with inherited thrombophilia had not been well studied [4]. It is usually considered in those with recurrent DVTs, multiple thrombophilic disorders and in factor V Leiden homozygotes [1]. There needs to be consistent evaluation of individuals on long-term anticoagulation to assess bleeding and assess risks versus benefits in treatment.
Current medications include [6]: 1) Heparin: works more quickly than warfarin does and is safe in pregnancy, but must be monitored closely due to the risk of excess bleeding. 2) Warfarin: Bleeding is the most common side effect of warfarin and it interacts with the metabolism of numerous other medications. 3) Dabigatran: It does not require the same monitoring that heparin and warfarin do but there is no reversal medication for excess bleeding. 4) Rivaroxaban: Currently FDA approved for the prevention of blood clots in certain people, but is not specifically approved for the treatment of blood clots. It can also interact with a number of medications and is known to cause recurrent GI bleed [7].
Newer medications like the factor X inhibitors for anticoagulation therapy allow patients to benefit from oral anticoagulation without the need for frequent monitoring or dose adjustment [7]. They however still have side effects like GI bleeding that can be potentially life-threatening; therefore the need for safer and more effective antithrombotic agents still clearly exists.
There is a continuous need for consistent evaluation of individuals on long-term anticoagulation to assess bleeding and assess risks versus benefits in treatment. The possibility of creating a therapeutic balance remains an important area of research and great concern in order to provide hemodynamic stability in patients with factor V Leiden mutation. We recommend that more studies should be done for a more reliable and better tolerated treatment.
| Conclusion | ▴Top |
Factor V Leiden remains the most common cause of hypercoagulable states and people with factor V Leiden thrombophilia have a significantly higher-than-average risk of developing venous thromboembolic disease than the general population. The case we presented above was diagnosed with factor V Leiden deficiency treated with different anticoagulants later presented with GI bleeding.
Management of factor V Leiden continues to be a challenge due to the fact that the current treatment regimen has not been able to effectively provide treatment without adverse effects. We remain hopeful that there will be continued research in this area and that newer and emerging treatments will help balance the risks and help us manage our patients more effectively.
| References | ▴Top |
- Bertina RM, Koeleman BP, Koster T, Rosendaal FR, Dirven RJ, de Ronde H, van der Velden PA, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature. 1994;369(6475):64-67.
doi pubmed - Rodeghiero F, Tosetto A. Activated protein C resistance and factor V Leiden mutation are independent risk factors for venous thromboembolism. Ann Intern Med. 1999;130(8):643-650.
doi - Kujovich JL. Factor V Leiden thrombophilia. Genet Med. 2011;13(1):1-16.
doi pubmed - Ornstein DL, Cushman M. Cardiology patient page. Factor V Leiden. Circulation. 2003;107(15):e94-97.
doi pubmed - Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):454S-545S.
- Factor V Leiden Definition - Diseases and Conditions - Mayo Clinic [Internet]. Mayoclinic.org. 2014. Available from: http://www.mayoclinic.org/diseases-conditions/factor-v-leiden/basics/definition/con-20032637.
- Turpie AG. Oral, direct factor Xa inhibitors in development for the prevention and treatment of thromboembolic diseases. Arterioscler Thromb Vasc Biol. 2007;27(6):1238-1247.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


