| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Original Article
Volume 3, Number 2, June 2014, pages 27-33
Retrospective Analysis of Heparin-Induced Thrombocytopenia Management at a Large Tertiary Hospital
Frank C. Passero, Jra, b, Marin Xaviera
aScripps Mercy Hospital, San Diego, USA
bCorresponding Author: Frank C. Passero Jr., Medical Education Department, 4077 5th Avenue, MER 35, San Diego, CA 92103, USA
Manuscript accepted for publication May 29, 2014
Short title: Heparin-Induced Thrombocytopenia Management
doi: https://doi.org/10.14740/jh157w
| Abstract | ▴Top |
Background: Heparin-induced thrombocytopenia (HIT) is a disease that is difficult to quickly and accurately diagnose. The 4T score calculation is often used to determine the probability of HIT in order to guide further work-up and therapeutics. Our study aims to assess current practices regarding the diagnosis and management of HIT, particularly in reference to the appropriateness and cost of work-up and initiation of heparin alternatives based on the 4T score.
Methods: A retrospective chart review was carried out on patients at Scripps Mercy San Diego for whom work-up had been pursued with HIT antibody test and/or serotonin release assay between May 2011 and May 2012. For each of these patients a 4T score assessing the probability of HIT was carried out based on available chart information.
Results: Of the 218 work-ups reviewed, 74% had a low pre-test probability of HIT and 53% occurred in the medical intensive care unit (ICU). Only five of the 218 work-ups and one of the 116 ICU patient work-ups resulted in a diagnosis of HIT. The cost of using heparin alternatives in patients without a final diagnosis of HIT was approximately $100,750 and the cost of pursuing serologic work-up in patients with a low 4T score was $33,360. Average optical density (OD) scores among patients with a low and intermediate 4T score did not reach the threshold value for positivity with values of 0.257 and 0.334, respectively. Patients in the high 4T score group had average OD values of 1.68, which is 5 above the threshold for a positive result and the probability of HIT being present did not reach 50% until the OD was above 1.40.
Conclusions: This study demonstrates the significant costs associated with HIT diagnosis and management at a large hospital. Implementing a clinical decision support system to mitigate inappropriate ordering of serologic studies and initiation of heparin alternatives may be cost-saving. Further prospective studies will need to be undertaken to test this hypothesis.
Keywords: Heparin-induced thrombocytopenia; Systems-based analysis; Heparin alternatives; Cost analysis
| Introduction | ▴Top |
Heparin is commonly used in hospitalized patients for the prevention and treatment of thrombosis. Despite the obvious benefits of unfractionated and low-molecular weight heparin for these indications, it is not without risks. Among the risks of heparin use is heparin-induced thrombocytopenia (HIT), an immune mediated disorder caused by binding of IgG antibodies to platelet factor 4 in the presence of heparin. This complex subsequently binds to and activates platelets leading to increased coagulation and thrombosis. Approximately 1-5% of patients on heparin develop HIT, although the incidence in patients treated with low-molecular weight heparin is lower than in patients treated with unfractionated heparin [1]. The consequences of HIT can be devastating and it can cause life-threatening thrombosis as well as severe skin necrosis. The presence of HIT is often a concern in medical and surgical patients and is often suspected when close laboratory monitoring reveals a decline in platelet count. A 4T scoring system has previously been developed using clinical and laboratory data to assign patients a low, intermediate or high pre-test probability of HIT. When HIT is strongly suspected, heparin is typically discontinued and a heparin alternative is initiated pending further serologic work-up by serotonin release assay and ELISA anti-PF4 antibody testing. However, the diagnosis of HIT is complex and requires integration of laboratory data such as timing and severity of thrombocytopenia, as well as clinical data such as new thrombosis and exclusion of other more likely causes for thrombocytopenia such as sepsis. The indications for additional laboratory testing and initiation of heparin alternatives in cases of suspected HIT must take into account the above clinical-pathologic factors [2]. The potential for inappropriate and excessive laboratory work-up and use of heparin alternatives for HIT is a concern given the above issues [3]. Formal hematology consultation is often needed to guide management and therapy. Additionally, the use of heparin alternatives and further serologic work-up is not without significant financial cost. It is important to assess whether laboratory work-up for HIT is being ordered appropriately and if heparin alternatives are being used in a manner that maximize patient benefit and reduce potential harms. We conducted a retrospective chart review at our large tertiary care hospital in order to better define current practices, assess the appropriateness of work-up and management, and determine if there are opportunities to optimize diagnosis and cost-effective treatment of HIT.
| Materials and Methods | ▴Top |
Patient data
A retrospective chart review was carried out on patients at Scripps Mercy San Diego, a two-campus 700+ bed hospital including a level-1 Trauma Center, for whom work-up for HIT had been pursued between May 2011 and May 2012. The protocol was approved by the Scripps Institutional Review Board (IRB # 11-5776). The database query searched for patients for whom the HIT antibody serum test (HIT Ab) and/or the serotonin release assay (SRA) had been ordered. Some patients had been tested with the above studies on multiple occasions; however, data in these instances were only used for studies performed more than 3 months apart. Additional data obtained included the patient’s age, gender, the primary type of inpatient service they were admitted under (cardiovascular surgery, orthopedic surgery, general surgery, surgical ICU, medical ICU and medical wards), if HIT was diagnosed by either positive SRA or hematology consultant, whether the patient was initiated on heparin alternative, the type and duration of heparin alternative utilized, whether hematology consultation was obtained and patient survival to discharge.
4T score
The chart review utilized records to retrospectively calculate each patient’s 4T clinical probability score for HIT, a scoring mechanism that has been validated to evaluate the probability of HIT being present [4]. Physician notes, laboratory data and radiologic data were used to determine the timing and degree of platelet fall, exposure to heparin and/or heparin alternatives, presence of thrombotic sequelae and the presence of other diagnoses that might contribute to thrombocytopenia.
HIT antibody
The HIT antibody, PF4 IgG/IgM/IgA by ELISA test ordered on patients at Scripps Mercy is performed through ARUP labs and is a semi-quantitative enzyme-linked immunosorbent assay. Results are reported as optical density (OD) units with a value of 0.399 OD units or less considered a negative test.
Serotonin release assay
The serotonin release assay (SRA) is performed through Quest Diagnostics. It is a functional assay measuring heparin-dependent platelet activation. Serum taken from the patient is incubated with donor platelets containing radioactive 14C-serotonin and heparin. If antibodies are present in the patient, they will activate donor platelets and release radio-labeled serotonin from the platelets will be detectable on the assay. A greater than 20% release of the 14C-serotonin is considered a positive test. Different concentrations of heparin are used and the high-dose heparin must reduce the percent release obtained with low-dose heparin by at least 50% in order to demonstrate that the platelet activation is heparin dependent.
Statistical analysis
Data were analyzed using Fisher’s exact test for low-frequency events (n < 5), using a P-value cut-off of < 0.05 for significance.
| Results | ▴Top |
Demographic data and 4T scores
Based upon the query criteria, 214 individual patient records were available for review and of these there were 218 separate incidents that met the inclusion criteria for work-up of HIT. The age range of patients was 19 - 97 years old with the average age being 66 years old. One hundred seventeen patients (54%) were male. Among the patient work-ups, 216 HIT Ab tests and 56 SRA tests were performed. One hundred sixty-one (73.8%) of these work-ups fell into the low 4T score category, 49 (22.5%) of work-ups were in the intermediate 4T score category and eight patients (3.7%) were in the high 4T score category.
HIT antibody test results and OD scores
HIT was formally diagnosed in five patients (2.3%). Three patients were diagnosed by positive SRA results and two patients were diagnosed by the hematology consultant. Of the patients diagnosed with HIT, one was in the low 4T score category (0.62% of those patients), none were in intermediate 4T score category and four were in the high 4T score category (50% of those patients).
The HIT Ab was positive in 43 of the 216 incidents in which it was ordered. By 4T score, 25 patients (15.63%) in the low 4T score group, 12 patients (25%) in the intermediate score group and six patients (75%) in the high probability 4T score group had a positive HIT Ab. Of particular note, none of the patients in whom the HIT Ab was negative were diagnosed with HIT nor did they have a positive SRA. In addition to evaluating whether the HIT Ab was positive or negative, the average OD values of HIT Ab results were calculated for each 4T score. Our patients in the low and intermediate 4T group had OD values of 0.257 and 0.334, respectively (Table 1). Both of these values are below the threshold for a positive result. Patients in the high 4T score group had average OD values of 1.68, which is five times the threshold for a positive result.
 Click to view | Table 1. HIT Diagnosis, Test Results and Heparin Alternative Use by Clinical 4T Score |
As can be seen in Table 2, only patients with OD values greater than 2.0 had HIT confirmed by SRA testing. Only patients who had an SRA result were included in this analysis. There were two patients that were diagnosed by hematology/oncology consultants as having HIT without having confirmatory SRA testing and their OD values were 0.868 and 0.882.
 Click to view | Table 2. OD Cut-Offs and Presence of HIT |
HIT diagnosis and work-up by service type
Five patients in this study were diagnosed with HIT, representing 2.3% of all work-ups pursued. Within the study database, patients were further classified based upon the primary service they were on during the work-up for HIT. Patients on medical services accounted for the majority (80.7%) of work-ups for HIT. Overall, the distributions of low, intermediate and high 4T scores were similar in the surgical and medical groups (Fig. 1). The majority (approximately 74%) of patients on surgical and medical services had a low 4T score. HIT work-ups in medical ICU patients accounted for 53% of the total work-ups and the second largest percentage of work-ups was in medical patients on wards (28%).
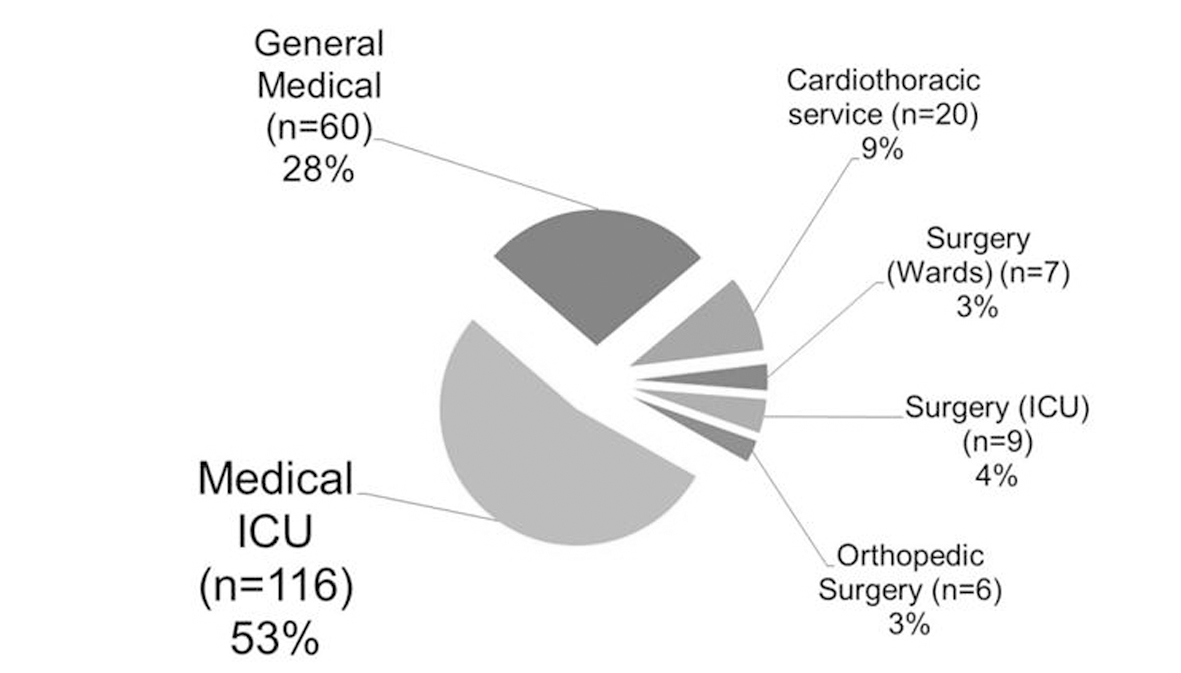 Click for large image | Figure 1. HIT work-up by service type. Percentage of patients undergoing work-up for HIT based on what service they were on. |
Use of heparin alternatives
The types of heparin alternatives used in patients in this study were argatroban, fondaparinux and bivalirudin. Among the 176 medical patients, 21 patients were started on heparin alternatives, 18 of whom were started on heparin alternatives in the absence of a final diagnosis of HIT. There were no patients in the surgical groups that were started on heparin alternatives in the absence of HIT being the final diagnosis (Fig. 2). The difference between surgical and medical groups in this regard was statistically significant (P = 0.0395 by Fisher’s exact test). Interestingly, nine out of the 176 medical patients were started on heparin alternatives despite having a low 4T score. The most common heparin alternative used was argatroban which was used in 22 of the 23 patients on heparin alternatives. The average duration was 6.28 days and median duration was 3.5 days on heparin alternative in patients without HIT. The cumulative total duration of heparin alternative therapy in patients without HIT was 113 days.
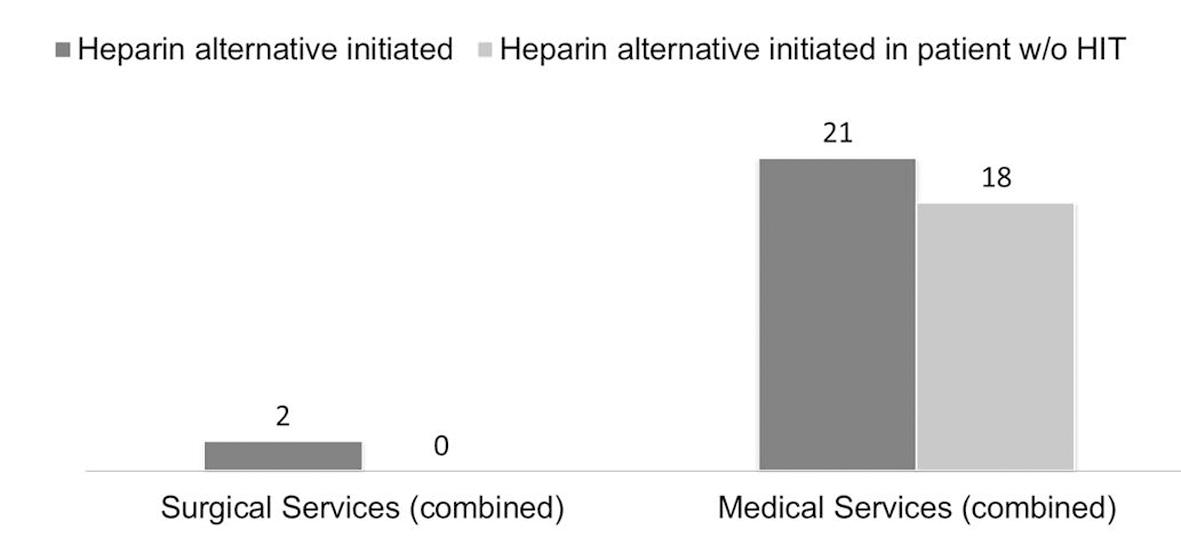 Click for large image | Figure 2. Use of heparin alternative by service type comparing medical and surgical services (P-value = 0.0395). |
Hematology consultation
All of the surgical patients in whom a heparin alternative was started had a hematology consult. In contrast, only 11 of 21 (52%) of the medical service patients in whom a heparin alternative was started had hematology involved; however, this difference was not statistically significant (P = 0.48 by Fischer’s exact test). All of the patients who were diagnosed with HIT had a/an hematology/oncology consult.
Morbidity and mortality
Overall, among the 214 patients in this study the survival to discharge was 79%. In the five patients diagnosed with HIT the survival to discharge was 100%. In patients without HIT who had been treated with a heparin alternative the survival to discharge was 78%, which is similar to the overall survival rate. There additionally were no reported adverse clinical events related to major bleeding found in patients without HIT treated with heparin alternatives.
Cost analysis
At our institution, the average cost of an HIT Ab test is approximately $150 and the SRA test is $260. Among patients at Mercy with a low 4T clinical score, the annual total cost savings of not performing the HIT Ab or the SRA would have been $33,360. The average estimated cost of patients without HIT who were treated with argatroban is $100,750 based upon a starting dose of 2 µg/kg/min in an average 70 kg individual and a price of $1,261.23 per 250 mg vial.
| Discussion | ▴Top |
In our study population, HIT was diagnosed in only 2.3% of patients undergoing work-up for it. In previously published studies [2, 5] the incidence of HIT diagnosis was between 3% and 17%. These studies also demonstrated a lower percentage of low 4T scores than seen in our study, suggesting that in our hospital over-ordering of diagnostic studies and unnecessary work-up for HIT is occurring. In our study, medical services (ICU and wards services combined) accounted for a statistically significant larger number of HIT work-ups and use of heparin alternatives in patients without HIT compared to surgical services (P-value < 0.05 by Fisher’s exact test). The majority of these work-ups were being carried out in ICU patients, a population which has previously been shown to have an already low pre-test probability of HIT based upon the higher likelihood of other etiologies (e.g. sepsis) contributing to thrombocytopenia in this group. The fact that only one out of the 116 ICU patients truly had HIT corroborated previous data that showed that the probability of HIT in an ICU patient being worked up for it is approximately 1 in 100 [6]. Additionally, the majority of patients treated with heparin alternatives (70%) in our study were ICU patients. This finding corroborates other studies [6, 7] which have found a high utilization of heparin alternatives to treat suspected HIT in the ICU, despite the low pre-test probability of HIT being a diagnosis in that setting.
In our patient population, the negative predictive value of a negative HIT Ab test in low and intermediate 4T groups was very high at 96% and 100% respectively. Conversely, the positive predictive value of a positive HIT Ab test in the high 4T group was 66.7%. These results are similar to results published by Bryant et al in which the positive predictive value of a positive HIT Ab test in low and high probability 4T score groups were 0% and 80% respectively [5]. In contrast to the Bryant et al study as well as data from Lo et al [4], none of the patients in our study with an intermediate 4T score had a positive SRA or were diagnosed with HIT. Of particular note, none of the patients with a negative HIT Ab in any of the 4T categories were diagnosed with HIT, indicating that a negative HIT Ab is a useful tool in excluding the diagnosis of HIT even in those patients in whom it is highly suspected.
A prior study by Warkentin et al demonstrated that the quantitative value of the HIT Ab result has prognostic indications in determining the probability of HIT, with higher OD values correlating with increased probability of HIT. In that study the probability of HIT being ≥ 50% does not occur until the OD reached a value of 1.40 or greater [8]. Our study corroborated these findings, demonstrating that the probability of HIT being present was 50% when OD was > 1.4 and 75% when OD was > 2.0. There was an association between higher 4T scores and OD values, as evidenced by the fact that only the average OD values in the high 4T score group were positive as opposed to an average OD value that correlated with a negative result in the low and intermediate 4T score groups. In addition there was a linear trend (R2 = 0.1139) towards higher OD values for higher 4T scores (Fig. 3).
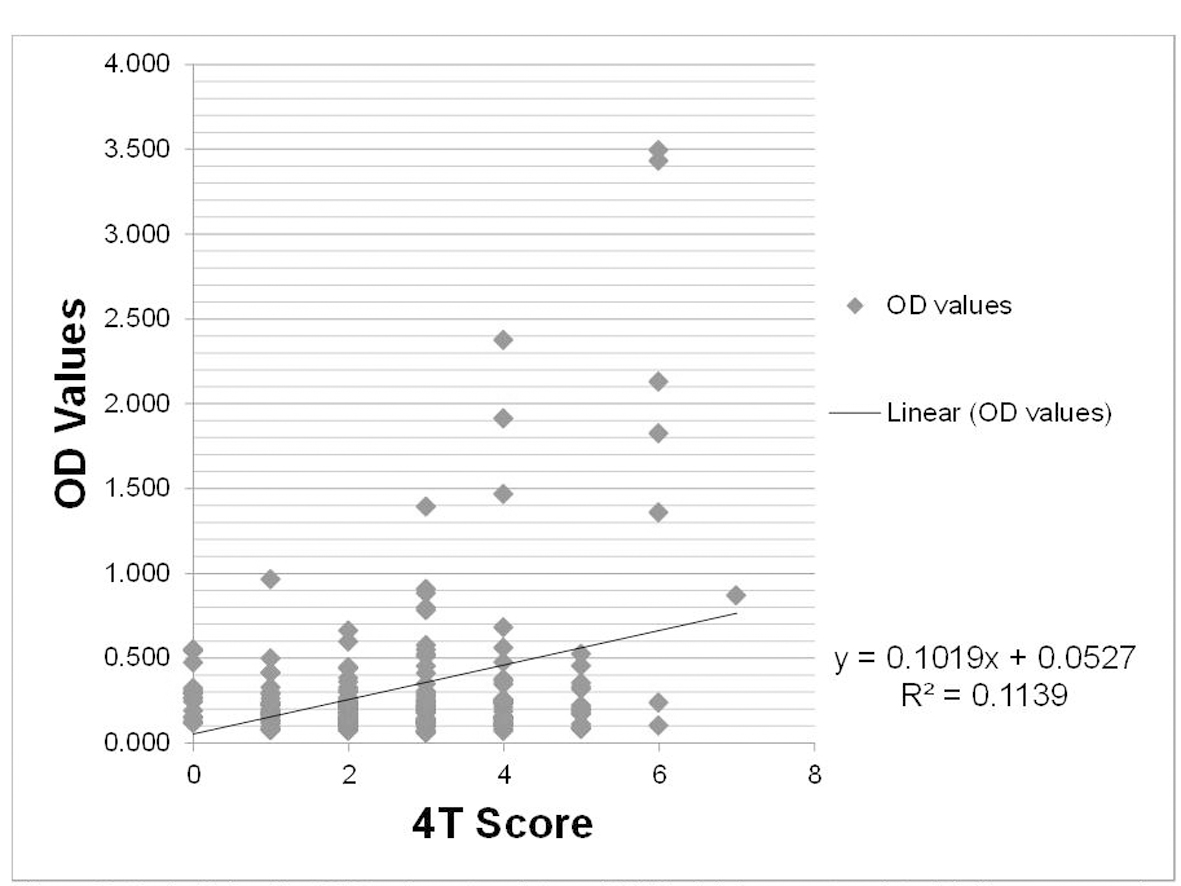 Click for large image | Figure 3. OD values by 4T score. OD values (y-axis) and clinical 4T score (x-axis) with linear regression plot showing increasing OD values with increasing clinical 4T score. |
Previous studies have correlated 4T scores with OD values as well as risk of thrombosis in HIT [9-11], and there have been suggestions that higher OD cut-off values to increase the specificity of the HIT Ab test would be beneficial in increasing the accuracy of diagnosis and more appropriate management of HIT [12]. Future prospective studies will need to delineate how use of 4T score and OD value results in this way will implicate the management of HIT.
Mortality was not increased among patients treated with heparin alternatives and there were no reported adverse effects such as major bleeding. The lack of adverse effect is likely due to our institution’s pharmaceutical policies on heparin alternatives and protocols for their safe usage. The median duration of 3.5 days in patients without HIT treated with heparin alternatives also likely reflects the fact that heparin alternatives were appropriately discontinued once HIT was excluded as a diagnosis once the results of HIT Ab or SRA returned with a negative result. However, when taking cost into consideration, the use of heparin alternatives in patients that did not have HIT was not inconsequential. The estimated annual cost of treating patients with argatroban in the absence of HIT was approximately $100,000. This equates to $1,000 per day per patient which is similar to the estimated daily cost of argatroban by Linkins et al in 2011 [1]. Additionally, the work-up of HIT in patients with a low 4T was associated with a cost of approximately $33,000.
This study was limited by the fact that it was a retrospective study and information from chart records was used to determine 4T scores for patients. Although a careful analysis of chart documents was carried out, missing information may have resulted in inaccurate 4T score calculation. For example, a patient may have been recently hospitalized at a different institution and received heparin-containing products without a notation of this being made in the chart. This would result in a lower calculated 4T score since the assumption in this case would be made that the patient had not previously received heparin. Additionally, this study was performed at a single institution and the generalizability of our results may be limited. Only 56 patients in our study had an SRA ordered. Of the patients without an SRA ordered, 14 had a positive HIT Ab and the majority of those had an OD value between 0.4 and 1.0. Two of those patients were diagnosed by the hematology consultant as having HIT on clinical basis and presence of HIT Ab being positive. The lack of SRA results in all of the patients being worked up for HIT limits the probability analysis of HIT Ab scores.
Overall, our study highlights current practices at a large hospital. It demonstrates that there are potential areas for improvement in both the diagnosis and management of HIT. It appears that overuse of HIT Ab and SRA studies in patients with low 4T scores, especially in the ICU setting, could be curtailed. Additionally, more appropriate use of heparin alternative could potentially be cost-saving. One future area of research that could address these issues would be to institute a computer-based clinical decision support system incorporating the 4T score at the point of ordering studies for HIT or initiating heparin alternatives and assess how the management of HIT is affected. Additionally, this study emphasizes the need for further research into the utility of incorporating OD scores into the diagnosis and management of HIT.
Conflict of Interest
Marin Xavier, MD: Honoraria for Cephalon/Teva, Allos/Spectrum, Seattle Genetics, Eisai, Celgene, Incyte. None of these companies has a direct interest in the topic of this manuscript. Frank C. Passero Jr., MD: No potential conflicts of interest to disclose.
| References | ▴Top |
- Linkins LA, Dans AL, Moores LK, Bona R, Davidson BL, Schulman S, Crowther M. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e495S-530S.
- Warkentin TE. How I diagnose and manage HIT. Hematology Am Soc Hematol Educ Program. 2011;2011:143-149.
doi pubmed - Cuker A. Heparin-induced thrombocytopenia (HIT) in 2011: an epidemic of overdiagnosis. Thromb Haemost. 2011;106(6):993-994.
doi pubmed - Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A. Evaluation of pretest clinical score (4 T's) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4(4):759-765.
doi pubmed - Bryant A, Low J, Austin S, Joseph JE. Timely diagnosis and management of heparin-induced thrombocytopenia in a frequent request, low incidence single centre using clinical 4T's score and particle gel immunoassay. Br J Haematol. 2008;143(5):721-726.
doi pubmed - Crowther MA, Cook DJ, Albert M, Williamson D, Meade M, Granton J, Skrobik Y, et al. The 4Ts scoring system for heparin-induced thrombocytopenia in medical-surgical intensive care unit patients. J Crit Care. 2010;25(2):287-293.
doi pubmed - Skrupky LP, Smith JR, Deal EN, Arnold H, Hollands JM, Martinez EJ, Micek ST. Comparison of bivalirudin and argatroban for the management of heparin-induced thrombocytopenia. Pharmacotherapy. 2010;30(12):1229-1238.
doi pubmed - Warkentin TE, Sheppard JI, Moore JC, Sigouin CS, Kelton JG. Quantitative interpretation of optical density measurements using PF4-dependent enzyme-immunoassays. J Thromb Haemost. 2008;6(8):1304-1312.
doi pubmed - Zwicker JI, Uhl L, Huang WY, Shaz BH, Bauer KA. Thrombosis and ELISA optical density values in hospitalized patients with heparin-induced thrombocytopenia. J Thromb Haemost. 2004;2(12):2133-2137.
doi pubmed - Weiss BM, Shumway NM, Howard RS, Ketchum LK, Reid TJ. Optical density values correlate with the clinical probability of heparin induced thrombocytopenia. J Thromb Thrombolysis. 2008;26(3):243-247.
doi pubmed - Kim SY, Kim HK, Han KS, Kim I, Yoon SS, Park S, Kim BK. Utility of ELISA optical density values and clinical scores for the diagnosis of and thrombosis prediction in heparin-induced thrombocytopenia. Korean J Lab Med. 2011;31(1):1-8.
doi pubmed - Raschke RA, Curry SC, Warkentin TE, Gerkin RD. Improving clinical interpretation of the anti-platelet factor 4/heparin enzyme-linked immunosorbent assay for the diagnosis of heparin-induced thrombocytopenia through the use of receiver operating characteristic analysis, stratum-specific likelihood ratios, and Bayes theorem. Chest. 2013;144(4):1269-1275.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


