| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 2, Number 2, October 2013, pages 76-78
Hepatitis C Virus Associated Hemophagocytic Lymphohistiocytosis: Case Report and Literature Review
Daniel F. Peasea, c, Josy Mathewb
aDepartment of Medicine, Hennepin County Medical Center, Minneapolis, MN, USA
bDepartment of Hematology/Oncology, Hennepin County Medical Center, Minneapolis, MN, USA
cCorresponding author: Daniel F. Pease, Department of Medicine, Hennepin County Medical Center, 701 Park Avenue, Minneapolis, MN 55415, USA
Manuscript accepted for publication August 15, 2013
Short title: Hepatitis C Virus
doi: https://doi.org/10.4021/jh82w
| Abstract | ▴Top |
A 46-year-old male presented with 10 days of fatigue, jaundice, and bloody sputum. Past medical history was significant for chronic hepatitis C virus (HCV) infection, with viral load > 10 million copies by PCR. Lab work showed severe derangements of multiple organ systems including cytopenias, renal failure, and transaminitis; a bone marrow biopsy revealed hemophagocytosis. On hospital day three he was started on definitive treatment for hemophagocytic lymphohistiocytosis (HLH) consisting of etoposide and dexamethasone, with marked improvement in condition. An exhaustive workup for infectious, rheumatologic, and malignant secondary etiologies was negative. In addition, genetic testing did not reveal a primary defect. We therefore postulate his HLH to be associated with chronic untreated HCV infection, a previously unreported clinical scenario in the literature.
Keywords: Hemophagocytic lymphohistiocytosis; Hepatitis C virus; Hematologic malignancy
| Introduction | ▴Top |
Hemophagocytic lymphohistiocytosis (HLH) is a life-threatening illness from profound dysregulation and hyperactivity of the immune system, often leading to multi-organ failure and death without prompt treatment. The underlying pathology involves the inability to extinguish an antigen-stimulated response driven by the interaction of macrophages, CD4+ helper/CD8+ cytotoxic T cells, and NK cells [1, 2]. The condition is divided into cases with primary genetic defects in cell-mediated cytotoxicity and cases with secondary factors inciting the excessive immune response. Secondary causes are most commonly infectious, especially viral, and less often malignant or rheumatologic.
| Case Report | ▴Top |
A 46-year-old African-American male presented to clinic with 10 days of fatigue, jaundice, and bloody sputum. Past medical history was significant for chronic untreated hepatitis C virus (HCV) infection, genotype 1a, with viral load > 10 million IU/mL. On exam he appeared acutely ill, with conjunctival pallor, scleral icterus, and tachycardia. No hepatosplenomegaly was present. Lab work revealed multiple derangements including severe thrombocytopenia (platelet count 3000 mm3), anemia (Hb 7.4 g/dL), acute renal failure (Cr 10.8 mg/dL), transaminitis (AST 214, ALT 178 IU/L), and direct hyperbilirubinemia (22 mg/dL).
The patient was admitted to the intensive care unit for initiation of emergent hemodialysis. After no source of infection was identified, a suspicion for a malignant hematologic process led to a bone marrow biopsy on hospital day two, remarkable for hemophagocytosis (Fig. 1). Together with bicytopenia, hypertriglyceridemia (388 mg/dL), and hyperferritinemia (3914 ng/mL), this supported a preliminary diagnosis of HLH. On day three, definitive treatment was started with etoposide and dexamethasone, per the HLH-94 treatment protocol [3], with marked clinical and laboratory improvement over the proceeding 48 hours. Several days later, soluble CD25 levels returned elevated (> 6,500 U/mL), satisfying 5 of the 8 HLH-2004 diagnostic criteria [2].
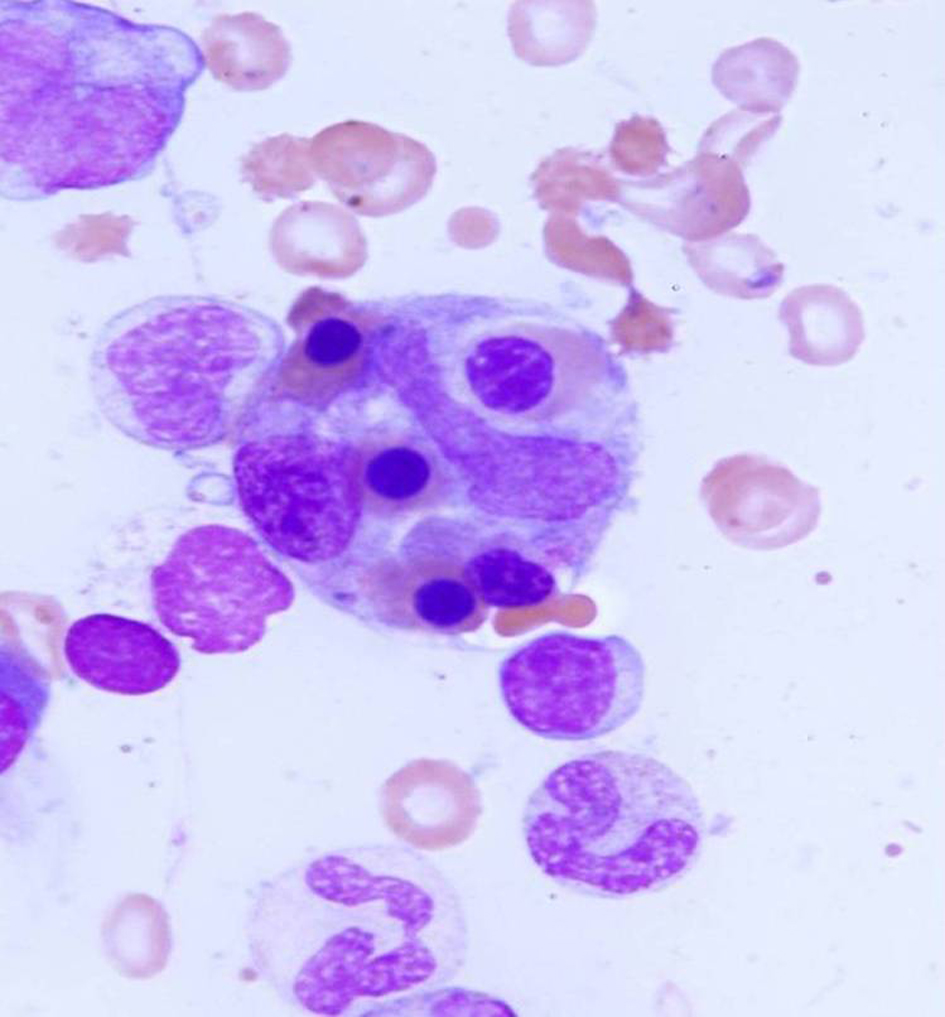 Click for large image | Figure 1. Bone marrow aspirate from the patient demonstrating numerous lymphocytes engulfed by a macrophage. |
An exhaustive workup for infectious, malignant, and rheumatologic secondary causes proved unrevealing. In addition, PCR-based testing for the five mutations accounting for nearly 100% of primary cases in North America (PRF1, MUNC13-4, STXBP2, STX11, and RAB27A) returned negative [2]. HCV infection remained as the only potential causative factor. The patient remains in remission 2 years post-treatment.
| Discussion | ▴Top |
The pathophysiology of HLH requires a potent stimulus of the immune system, followed by an inability to extinguish the consequent response. This is most commonly accomplished by viruses, with EBV and CMV the frequent culprits [1]. The association of hepatitis viruses with HLH also has precedence in the literature. While the context of HLH due to infection with hepatitis A or hepatitis B has been established [4, 5], the relationship with hepatitis C is more complex (Table 1). Several reports document co-infection with a separate strain of hepatitis virus in addition to hepatitis C [6, 7], while others detail a clinical picture of concurrent immune therapy and HCV as leading to HLH [8, 9]. However, we believe this is the first reported case of chronic HCV, without simultaneous co-infection or immunomodulatory therapy, as the lone inciting factor for HLH.
 Click to view | Table 1. Literature Review of HLH Cases Associated With HCV. |
The hypothesized relationship of chronic HCV and subsequent HLH holds several implications. The U.S has a large population of patients with chronic hepatitis C, estimated at 2.7 - 3.9 million, many undiagnosed [10]. With most untreated and harboring high viral loads as potential antigenic stimuli, we may recognize HLH caused by HCV more frequently. Patients with acute multi-organ dysfunction of unknown cause need evaluation for hepatitis C and increased suspicion for the inclusion of HLH in the differential diagnosis should testing prove positive.
When considering many autoimmune conditions, including cryoglobulinemia, thyroiditis, MPGN, and lymphomas, HCV is included in the differential as a possible inciting factor [11]. The proposed mechanism is presentation of both foreign HCV antigens and self-antigens to local dendritic cells, thus causing cross-reactivity and autoimmune disease. The accepted pathophysiology of HLH, a hyper-stimulated immune system, could be set in motion by such a reaction. Perhaps HLH needs to be added to the list of HCV-induced autoimmune conditions.
In addition, the risks and benefits of HCV treatment in this scenario become very complex. Interferon is the mainstay of treatment regimens outside of experimental contexts, and indeed interferon is one of several immunomodulating agents implicated in the “cytokine storm” of HLH [2]. Consequently, treatment of HCV in such a patient requires clarification, in view of the potential for immune stimulation from interferon therapy leading to relapse of HLH. That continued chronic immune system activation from the untreated hepatitis C viremia may itself lead to HLH relapse lends urgency to the issue. Our patient has yet to be treated for HCV due to the aforementioned risk of interferon therapy, but the discussion certainly would be revisited were his HLH to relapse.
Regardless of the decision to treat HCV, this is the first documented case of successful use of the HLH-94 treatment protocol in the context of HCV. The literature review reveals a variety of treatments in the four previously documented cases; unfortunately none of those patients survived. Our experience may be of guidance should similar cases arise in the future.
Declaration
The authors have no funding sources or conflicts of interest to report related to the manuscript.
| References | ▴Top |
- Filipovich AH. Hemophagocytic lymphohistiocytosis and other hemophagocytic disorders. Immunol Allergy Clin North Am. 2008;28(2):293-313, viii.
doi pubmed - Canna SW, Behrens EM. Making sense of the cytokine storm: a conceptual framework for understanding, diagnosing, and treating hemophagocytic syndromes. Pediatr Clin North Am. 2012;59(2):329-344.
doi pubmed - Trottestam H, Horne A, Arico M, Egeler RM, Filipovich AH, Gadner H, Imashuku S, et al. Chemoimmunotherapy for hemophagocytic lymphohistiocytosis: long-term results of the HLH-94 treatment protocol. Blood. 2011;118(17):4577-4584.
doi pubmed - Tuon FF, Gomes VS, Amato VS, Graf ME, Fonseca GH, Lazari C, Nicodemo AC. Hemophagocytic syndrome associated with hepatitis A: case report and literature review. Rev Inst Med Trop Sao Paulo. 2008;50(2):123-127.
doi pubmed - Aleem A, Al Amoudi S, Al-Mashhadani S, Siddiqui N. Haemophagocytic syndrome associated with hepatitis-B virus infection responding to etoposide. Clin Lab Haematol. 2005;27(6):395-398.
doi pubmed - Faurschou M, Nielsen OJ, Hansen PB, Juhl BR, Hasselbalch H. Fatal virus-associated hemophagocytic syndrome associated with coexistent chronic active hepatitis B and acute hepatitis C virus infection. Am J Hematol. 1999;61(2):135-138.
doi - Wu CS, Chang KY, Dunn P, Lo TH. Acute hepatitis A with coexistent hepatitis C virus infection presenting as a virus-associated hemophagocytic syndrome: a case report. Am J Gastroenterol. 1995;90(6):1002-1005.
pubmed - Tierney LM, Jr., Thabet A, Nishino H. Case records of the Massachusetts General Hospital. Case 10-2011. A woman with fever, confusion, liver failure, anemia, and thrombocytopenia. N Engl J Med. 2011;364(13):1259-1270.
doi pubmed - Akamatsu N, Sugawara Y, Tamura S, Matsui Y, Hasegawa K, Imamura H, Kokudo N, et al. Hemophagocytic syndrome after adult-to-adult living donor liver transplantation. Transplant Proc. 2006;38(5):1425-1428.
doi pubmed - Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo CG, Jewett A, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61(RR-4):1-32.
pubmed - Paroli M, Iannucci G, Accapezzato D. Hepatitis C virus infection and autoimmune diseases. Int J Gen Med. 2012;5:903-907.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


