| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Original Article
Volume 10, Number 2, April 2021, pages 64-70
ABO in Correlation to the Requirement of Mechanical Ventilation and Mortality in Critically Ill Patients With COVID-19
Rehab Y. Al-Ansaria, f , Abdulaziz Alshaerb, Aamer Al-Anazic, Nasser Al-Otaibic, Leena Abdallaa, Sufana Al-Tarrahd, Amal Shilashe, Nada Al-Zahranid
aAdult Hematology Unit, Internal Medicine Department, KFMMC, Dhahran 31932, Saudi Arabia
bCritical Care Department, KFMMC, Dhahran 31932, Saudi Arabia
cLaboratory Department-Blood Bank, KFMMC, Dhahran 31932, Saudi Arabia
dInternal Medicine Department, KFMMC, Dhahran 31932, Saudi Arabia
eInfection Control Department, KFMMC, Dhahran 31932, Saudi Arabia
fCorresponding Author: Rehab Y. Al-Ansari, Adult Hematology Unit, Internal Medicine Department, KFMMC, Dhahran 31932, Saudi Arabia
Manuscript submitted March 23, 2021, accepted April 6, 2021, published online April 27, 2021
Short title: ABO Types in COVID-19 Patients
doi: https://doi.org/10.14740/jh821
| Abstract | ▴Top |
Background: Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that was first discovered in December 2019 and turned to be pandemic in early March 2020. We aimed to describe the dominant ABO group and outcomes of critically ill patients (respiratory failure requiring mechanical ventilation and mortality) in a Saudi Arabian setting.
Methods: We conducted an observational, analytic cross-sectional, retrospective study in a tertiary care hospital. Around 90 candidates tested positive for COVID-19 were enrolled in this study during admission to critical care unit between May 2020 and September 2020. Blood group was detected in all patients included in the study during admission to critical care unit.
Results: In this study, data of 90 patients with COVID-19 admitted to critical care unit were collected. Some prevalent medical conditions were collected, in which hypertension (64.2%) and diabetes mellitus (58.9%) were the most reported comorbidities among patients and there was no significant difference between groups. Most of the sample had blood group of O (45.6%), while the least group was AB (5.6%). Patients with blood group of A/AB showed the highest mortality vs. group O/B (32% vs. 18.5%) with significant P value of 0.001. Patients of groups A/AB had higher risk for intubation than O/B groups (52.0% and 49.2%, respectively; confidence interval of 0.44 - 2.8 with insignificant P value of 0.055). Length of stay in critical care unit was significantly higher in group A/AB with a mean course of 18.20 days in comparison to group O/B with a mean course of 12.63 days (P = 0.033).
Conclusion: Our data indicate that critically ill patients with COVID-19 with blood group A/AB are at increased risk of mortality and length of stay in critical care unit, with insignificant requirement of mechanical ventilation when compared with patients with blood group O/B. Future larger studies are needed to validate and understand the underlying mechanisms.
Keywords: ABO blood grouping; COVID-19; Mechanical ventilation; Critically ill patients; Mortality; Length of stay
| Introduction | ▴Top |
Dealing with critically ill patients with coronavirus disease 2019 (COVID-19) is a great challenge especially with limitation of data. Underlying comorbidities such as obesity, age, cardiovascular disease, diabetes, hypertension, smoking and dyslipidemia may play a role in disease severity and its outcome. Furthermore, some reports suggested the relationship of ABO blood grouping to susceptibly to COVID-19 and others suggested the worse outcome in relation to one blood group rather than others. Wu et al reported that patients with blood group A were at higher risk to be infected by COVID-19; on the other hand, patients with blood group O were at lower risk, which goes with other studies [1, 2]. In a study by Dai, blood group A predisposed to COVID-19 severity as well as to hypertension and cardiovascular disease more than the other blood groups [3]. One study supported that patients with blood group A were at higher risk of respiratory failure from COVID-19 [4]. However, an association between ABO blood type and outcome of COVID-19 was assessed in five major hospitals in the state of Massachusetts and the result was against any relation between blood grouping and intubation or death [5]. On the other hand, the ethnicity and distribution of population with different blood groups may play a role. In Saudi Arabia population, a study showed that blood group O is predominant and group A is less frequent than in Western populations [6]. The main question behind this study is that the blood grouping has impact on requirement of mechanical ventilation and mortality in critically ill patients with COVID-19 in Saudi population. Therefore, we conducted a retrospective study in which we correlated the ABO group to patient outcome, length of stay (LOS) in critical care unit as well as the requirement of mechanical ventilation in uni-center study aiming for further multicenter national project.
| Materials and Methods | ▴Top |
An observational, analytic, cross-sectional, retrospective study was conducted in a tertiary care hospital (KFMMC, Dhahran, Saudi Arabia). Around 90 candidates tested positive for COVID-19 were enrolled in this study during admission to critical care unit between May 2020 and September 2020. Historical data about blood group and LOS in critical care unit as well as the requirement of mechanical ventilation and mortality were taken from the chart of all patients admitted to the intensive care unit (ICU). Blood grouping which was not drawn during admission was taken from patient medical records. ABO blood type at the local center as well as in other Saudi centers was done automatically by microplate method which basically determined the presence of corresponding antigens (anti-A and anti-B) [7].
Any adult patients, aged ≥ 18 years old, affected by COVID-19 admitted to the hospital ICU were considered as eligible for this study. On the other hand, COVID-19 negative cases and pediatric age group were excluded.
We collected the demographic data including age, sex, comorbidities as well as hospital course and data related to critical care unit admission as follows: LOS in ICU and LOS in hospital, APACHE II score, requirement and duration of mechanical ventilation, as well as laboratory parameters at baseline on admission to critical care unit, including white blood cell (WBC) count, hemoglobin (HG) level, lymphocyte count, neutrophil count, platelet (Plt) count, lactate dehydrogenase (LDH), C-reactive protein (CRP), fibrin, D-dimer and ferritin.
Patients and management
All critically ill patients with confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on nasopharyngeal and, if mechanical ventilation was required, another tracheal sample were included. The Saudi Critical Care Society COVID-19 Patient Critical Care Management Guideline in accordance with the Surviving Sepsis Campaign was followed.
We followed the WHO and NICE guidelines for critical care advice to use of a set escalation plan and utilized medical early warning score (e.g., NEWS2) that facilitate early recognition and escalation of treatment of the deteriorating patients (Table 1).
 Click to view | Table 1. Assessment and Guidance for COVID-19 Patient Critical Care Management |
Critical care admission and discharge were regulated according to the criteria and mechanical ventilation was decided by discretion of attending intensivist once the high flow nasal cannula and non-invasively administered oxygen was not enough to maintain the peripheral oximetry saturation > 94%. Patients were treated with sedation protocol propofol, benzodiazepine and narcotic. Protective lung strategy and proning was utilized whenever indicated. Whenever the patients were suitable for weaning with adequate level of consciousness, fraction of oxygen < 40%, positive end-expiratory pressure (PEEP) < 8 cm H2O and minimal tracheal secretion with moderate to strong cough, patients would be on pressure support of 8 cm H2O trail and if passed the criteria, they would be extubated. Enoxaparin (30 - 40 mg) was administered subcutaneously every 12 h as thromboprophylaxis. Continuous renal replacement therapy (CRRT) was utilized whenever medically indicated.
Blood group distributions (national and provincial)
The distribution of national and provincial ABO blood groups for Saudi papulation was obtained from previous researches at the level of eastern province and further wider to involve other provinces so called national as there is no real ABO blood group or hematology registry.
Outcomes
Our primary end point was to assess blood group and correlation with the requirement of mechanical ventilation in critically ill patients with COVID-19. Furthermore, our secondary end point was to assess blood group and correlation with mortality in critically ill patients with COVID-19.
The primary and secondary end points were chosen for the value of clinically relevant and indicative of disease severity that frequently occurs in critically ill patients with COVID-19. Moreover, given a smaller sample size, those factors can ensure reasonable power to our study.
Statistical analysis
Statistical analysis was done with STATA version 16 Statistical Analysis Software to analyze the baseline characteristics of the data and the correlations between the variables in the patients’ data. Mean and standard deviation as well as frequency and percent were used for description of data. T-test and analysis of variance (ANOVA) test were used for assessing the correlation between variables where correlation was significant when P value ≤ 0.05.
The study was approved by the Armed Forces Hospital Eastern Province Institutional Review Board (AFHER-IRB-2020-036). The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
In this study, data of 90 patients admitted with COVID-19 were collected. Most of the sample had blood group of O (45.6%), while patients with blood group of A represented 22.2% of the sample, blood group of B represented 26.7% and blood group of AB represented 5.6% (Fig. 1).
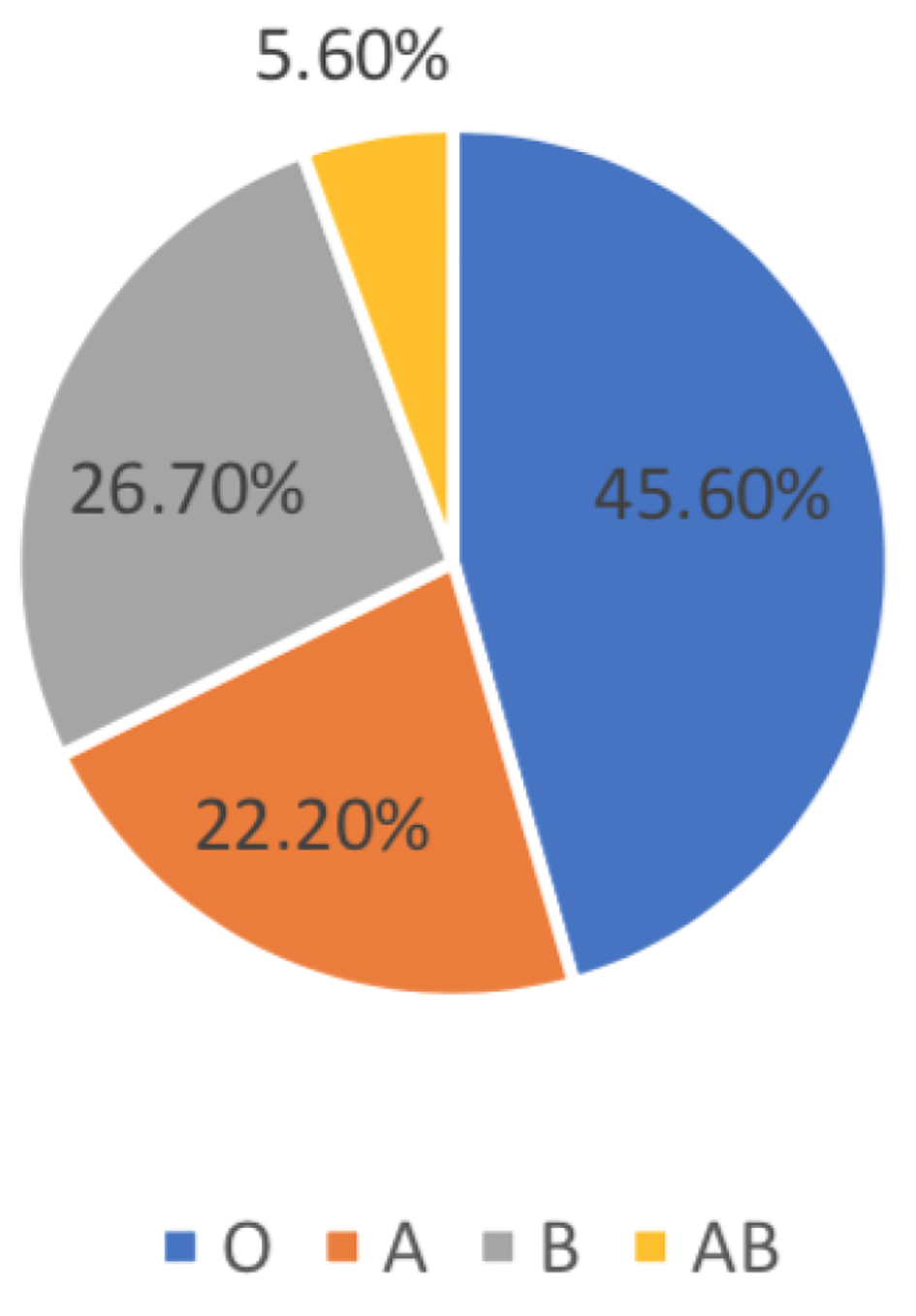 Click for large image | Figure 1. Distribution of blood groups. |
Our ICU cohort’s blood group distribution was not different from the national blood group distribution (P = 0.898) or the provincial blood group distribution (P = 0.888) (Table 2) [6].
 Click to view | Table 2. Comparison of Blood Group Distributions Between National and Provincial Blood Donor Data and ICU-Admitted Patients With COVID-19 |
Table 3 shows the differences of baseline demographic factors between blood groups. The mean age of the sample was 58.68 years old (standard deviation: 13.54). No significant difference was found among blood groups in terms of age; however, mean age of patients with O/B blood group was slightly higher than those with A/AB blood groups. Moreover, 68.8% of the sample was male and there is no significant difference between groups (P = 0.693). Some prevalent medical conditions were collected, in which hypertension (64.2%) and diabetes mellitus (58.9%) were the most reported comorbidities among patients and there is no significant difference between groups. Moreover, we compared the lab reports of patients finding that there were no significant differences between groups in most labs’ tests except for ferritin where patients with O/B groups had a significantly higher concentration of ferritin than those with A/AB blood groups (P = 0.036) (Fig. 2).
 Click to view | Table 3. Baseline Demographic Data and Laboratory Results of Patients |
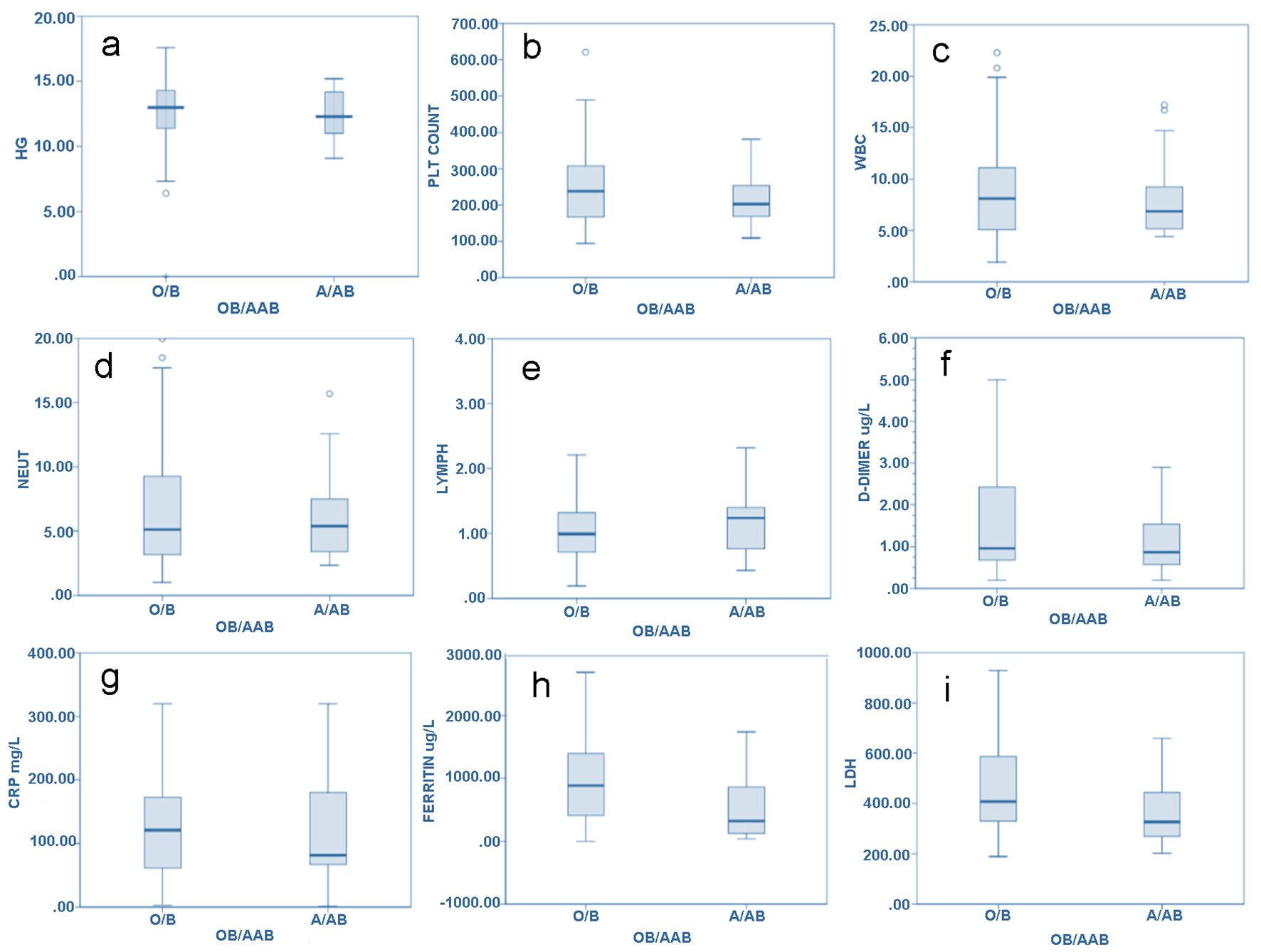 Click for large image | Figure 2. Box plots of clinical laboratory results and some serum inflammatory biomarkers. (a) hemoglobin; (b) platelet count; (c) white blood cell count; (d) neutrophil count; (e) lymphocyte count; (f) D-dimer; (g) C-reactive protein; (h) ferritin concentration; (i) lactate dehydrogenase. Sample size was 90 patients split into blood groups O/B and A/AB. |
Furthermore, the mean LOS in ICU was 13.7 days where A/AB groups (18.20 days) tended to have longer LOS in ICU than O/B groups (12.63 days) with a significant difference between groups (P = 0.00) which indicates a significant correlation between blood groups and LOS in ICU.
Almost half of the sample needed intubation during their hospitalization with a mean time of intubation of 7.34 days where patients with O/B blood groups (49.2%) needed intubation in lower frequency than those with A/AB blood groups (52%) which indicates that A/AB blood groups represent increasing risk for the need for intubation which is not significant. It was found in this study that 22.2% of sample died because of severe illness and there is a significant difference between blood groups in death rates where A/AB groups have the mortality of 32% compared to O/B blood groups with a mortality of 18.5% which indicates group of A/AB groups possess the risk factor of death by two times versus O/B blood groups which is significant. There is significant correlation between blood groups and death rates.
Within groups, we found that patients with AB were at higher risk for death because of COVID-19 than O group by 2.91 times (odds ratio (OR): 2.91, confidence interval (CI): 0.4338 - 19.69, P = 0.27) and B group had higher risk of about two times over O (OR: 1.94, CI: 0.54 - 6.8, P = 0.303) while patients of A had risk for deaths by about 2.4 times than O group (OR: 2.5, CI: 0.688 - 9.08, P = 0.163). Moreover, the baseline characteristic APACHE II score showed insignificant difference in both groups with predicted mortality of total sample of 22% compared to our mortality data of 22.2% (Table 4).
 Click to view | Table 4. Clinical Outcomes Between Groups O/B and Groups A/AB |
Moreover, we found that length of hospitalization increased the risk for both the need for mechanical ventilation and mortality; however, no significant difference was found between blood groups (Fig. 3).
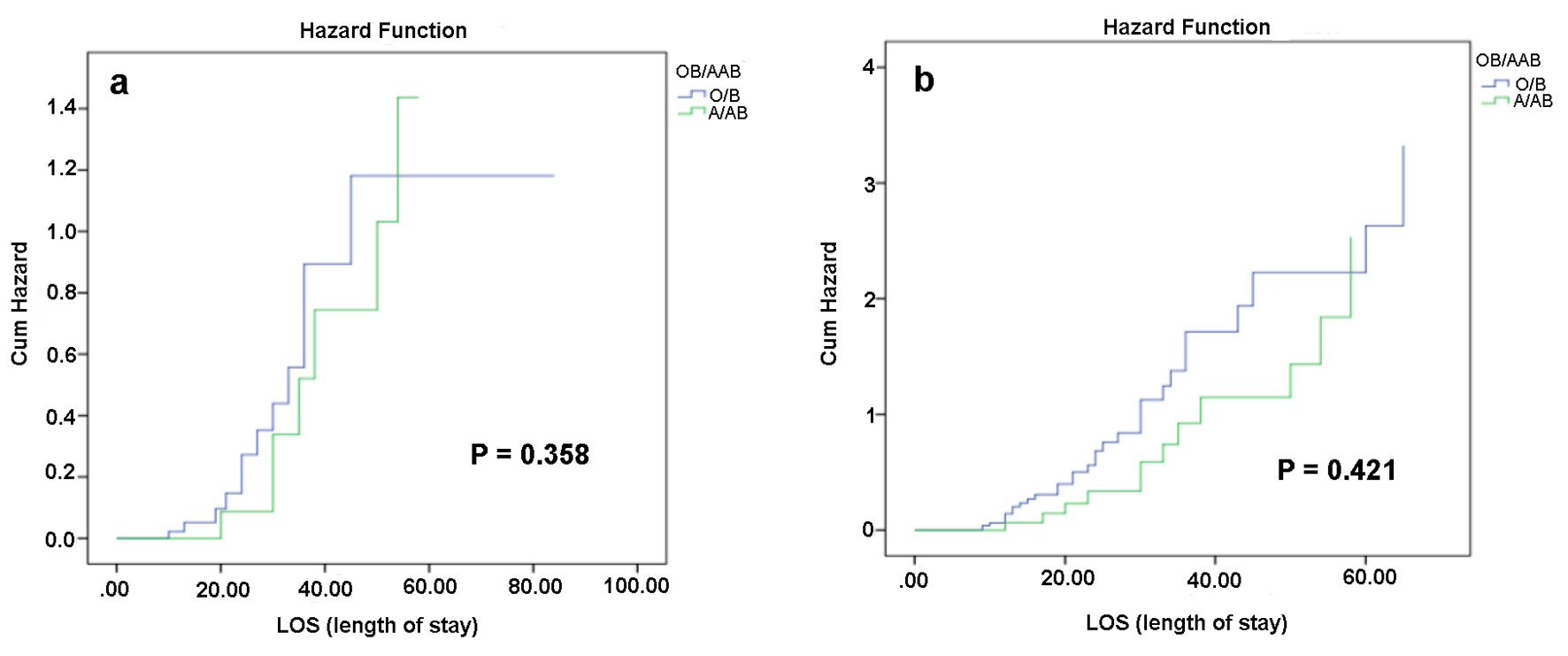 Click for large image | Figure 3. Cumulative hazards of length of stay and blood factors on both mortality and need for intubation. Both risk of mortality and need for intubation increase with the increased length of stay in all blood groups with no significant difference. |
| Discussion | ▴Top |
We need better understanding of the novel virus causing COVID-19in order to reduce its impact on the world. In this study, we investigated whether blood type is relevant for need for mechanical ventilation and/or morality. Therefore, we retrospectively reviewed clinical data of 90 critically ill patients who were positive for the new virus with the mean age of 58 years old (13.9) which is in agreement with most of studies conducted over patients with COVID-19 where mean age of patients with COVID-19 ranged between 53 and 73 years [8-12]. Moreover, in this study, we found that people with blood groups O, A, B and AB were 45.6%, 22.2%, 26.7% and 5.6%, respectively. For the AB group sample, it goes in coherence with the national (4.1%) and regional (4%) prevalence which is at higher risk for COVID-19 while 45.6% of the sample was of O blood group. This is in agreement with the study of Latz et al who found that 45.5% of infected patients were of blood type O while 15.6% were of blood type B and 4.7% were of blood type AB [5]. Zietz et al found that 47.2% of patients with COVID-19 were of blood type O and AB was the least blood type of 4.3% [11]. Zhao et al found that 33.84% of patients were of blood type O and only 9.1% were of AB [13]. However, we should consider that studies showed that prevalence of AB was significantly lower than O [14], therefore, this could be normal distribution of ABO among random sample while some studies which compared between normal population and patients with COVID-19 found that prevalence of group O was lower in patients than normal population [5]. Moreover, among different ABO, we did not find significant difference between age of patients and the ABO type, which is in agreement with other studies [1, 8, 11]. Furthermore, we found that hypertension and diabetes mellitus were the most prevalent conditions found in COVID-19 patients, which is similar to results of other studies [1, 8, 9].
Moreover, we found that ABO had no significant effect on need for intubation or mechanical ventilation days while there is tendency of A/AB group to have higher incidence of ICU LOS and hospitalization compared to O/B groups. However, we found that half of the sample needed intubation and mean lengths of hospitalization, intubation and ICU were 19.2, 7.34 and 13.7 days. Patients in our study had longer LOS, intubation and ICU stay, while in study of Latz et al, only 8.7% of patients needed intubation; however, they agreed with our results that ABO do not affect the need for intubation [1]. In addition, Zietz et al found that only 3.2% of patients needed intubation with no significant correlation with ABO groups [11]. Moreover, Hoiland et al found that mean length of hospitalization and ICU stay were higher in patients with groups of A/AB than those with O/B which matches with our result [8].
In terms of mortality, we found a correlation between ABO and mortality rate where O/B had the lowest mortality while A/AB had the highest mortality; besides AB had higher risk for mortality when compared with O group by almost eight times. This is in agreement with the study by Zhao et al, who found that 41.26% of deaths were A group while 25.24% were O group and 9.22% were AB, and blood group A was associated with higher risk of death compared with non-A groups by 1.48 times while blood group O was associated with lower risk of death compared with non-O groups [5]. Moreover, this is in agreement with previous studies conducted for other SARS infection including the study by Cheg et al who reported that SARS-CoV infection and mortality could be differentiated by ABO blood group [11]. However, these results were in contrast with the results of Latz et al who did not find any correlation between ABO groups and mortality in patients with COVID-19 [14].
Furthermore, in this study, we did not find an association between any of these lab tests and blood group; however, some points should be taken into consideration. When we compared between A/AB which had the highest mortality and O/B which had the lowest mortality, we found that group of A/AB had lower HG, D-dimer, CRP, low-density lipoprotein (LDL) and higher Plt count, WBC, neutrophile and lymphocyte counts than O/B group which was not significant. Surprisingly, ferritin was significantly higher in A/AB compared to O/B group with P value of 0.036. Hoiland et al found that patients with groups A/AB had higher WBCs, CRP, ferritin and D-dimer than groups of O/B [8].
This study has some limitations that may affect the reliability of study. The first limitation is small sample size because this is a uni-center critical care unit study looking for further multicenter study with larger sample size. The second limitation is, even we standardize the baseline characteristic feature and APACHE II score for both groups, other co-founder and biologic mediator could play roles in COVID-19 outcome which is not yet well known to us rather than ABO blood group. Moreover, the third limitation is that it is a retrospective analysis of observational data, therefore causality cannot be determined.
In conclusion, we found an evidence for associations between ABO and mortality in COVID-19 patients where patients with ABO type of A/AB have the highest mortality rate and tendency of increased hospital/critical care LOS among other ABO types. However, we did not find association between ABO and need for intubation/mechanical ventilation days among both groups. Our results add further evidence to the previously discovered associations between blood types and COVID-19. More investigation is needed to explain how ABO affects mortality in patients with COVID-19.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Rehab Y. Al-Ansari wrote proposal, obtained IRB and wrote manuscript. Abdelaziz Alshaer wrote patient management part as first reviewer of the manuscript. Sufana AL-Tarrah contributed to data collection and reviewing. Aamer Al-Anazi wrote blood bank aspect in the study as second reviewer. Nasser Al-Otaibi contributed to data collection and reviewing. Leena Abdalla helped in designing the study as reviewer. Amal Shilash wrote result part and statistic task. Nada Al-Zahrani contributed to data collection and reviewing.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Wu Y, Feng Z, Li P, Yu Q. Relationship between ABO blood group distribution and clinical characteristics in patients with COVID-19. Clin Chim Acta. 2020;509:220-223.
doi pubmed - Zhao J, Yang Y, Huang HP, Li D, et al. Relationship between the ABO Blood Group and the COVID-19 susceptibility. medRxiv. 2020.
doi - Dai X. ABO blood group predisposes to COVID-19 severity and cardiovascular diseases. Eur J Prev Cardiol. 2020;27(13):1436-1437.
doi pubmed - Pourali F, Afshari M, Alizadeh-Navaei R, Javidnia J, Moosazadeh M, Hessami A. Relationship between blood group and risk of infection and death in COVID-19: a live meta-analysis. New Microbes New Infect. 2020;37:100743.
doi pubmed - Latz CA, DeCarlo C, Boitano L, Png CYM, Patell R, Conrad MF, Eagleton M, et al. Blood type and outcomes in patients with COVID-19. Ann Hematol. 2020;99(9):2113-2118.
doi pubmed - Bashwari LA, Al-Mulhim AA, Ahmad MS, Ahmed MA. Frequency of ABO blood groups in the Eastern region of Saudi Arabia. Saudi Med J. 2001;22(11):1008-1012.
- Standards for blood banks and transfusion services. 31st edition. American Association of Blood Banks. ISBN-13: 978-1563959585. ISBN-10: 1563959585.
- Hoiland RL, Fergusson NA, Mitra AR, Griesdale DEG, Devine DV, Stukas S, Cooper J, et al. The association of ABO blood group with indices of disease severity and multiorgan dysfunction in COVID-19. Blood Adv. 2020;4(20):4981-4989.
doi pubmed - King CS, Sahjwani D, Brown AW, Feroz S, Cameron P, Osborn E, Desai M, et al. Outcomes of mechanically ventilated patients with COVID-19 associated respiratory failure. PLoS One. 2020;15(11):e0242651.
doi pubmed - Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, Wang F, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA. 2020;323(16):1582-1589.
doi pubmed - Zietz M, Zucker J, Tatonetti NP. Associations between blood type and COVID-19 infection, intubation, and death. Nat Commun. 2020;11(1):5761.
doi pubmed - Canizalez-Roman A, Campos-Romero A, Castro-Sanchez JA, Lopez-Martinez MA, Andrade-Munoz FJ, Cruz-Zamudio CK, Ortiz-Espinoza TG, et al. Blood Groups distribution and gene diversity of the ABO and Rh (D) Loci in the Mexican population. Biomed Res Int. 2018;2018:1925619.
doi pubmed - Zhao J, Yang Y, Huang H, Li D, Gu D, Lu X, Zhang Z, et al. Relationship between the ABO Blood Group and the COVID-19 Susceptibility. Clin Infect Dis. 2020.
doi - Cheng Y, Cheng G, Chui CH, Lau FY, Chan PK, Ng MH, Sung JJ, et al. ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA. 2005;293(12):1450-1451.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


