| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 12, Number 6, December 2023, pages 272-276
Peripheral T-Cell Lymphoma in a Patient Previously Diagnosed With Sarcoidosis
Sanjay V. Menghania, b, g, h , Jessica P. Diaz-Hansona, g, Alex Heimbignerc, d, Chelby Wakefieldd, e, Deborah Fuchsc, d, Candace Y. Revelesc, d, Catherine Spierc, d, Akshay Amaranenid, e, f, Abhijeet Kumard, e, f
aUniversity of Arizona College of Medicine - Tucson, Tucson, AZ, USA
bMedical Scientist Training MD-PhD Program, University of Arizona College of Medicine - Tucson, Tucson, AZ, USA
cDepartment of Pathology, University of Arizona College of Medicine - Tucson, Tucson, AZ, USA
dBanner Health, Tucson, AZ, USA
eDivision of Hematology and Oncology, Department of Medicine, University of Arizona College of Medicine - Tucson, Tucson, AZ, USA
fUniversity of Arizona Cancer Center, University of Arizona College of Medicine - Tucson, Tucson, AZ, USA
gThese authors contributed equally to this work.
hCorresponding Author: Sanjay V. Menghani, UA College of Medicine MD/PhD Program, PO Box 210202, Tucson, AZ 85721-0202, USA
Manuscript submitted July 28, 2023, accepted September 19, 2023, published online December 9, 2023
Short title: PTCL Previously Diagnosed With Sarcoidosis
doi: https://doi.org/10.14740/jh1173
| Abstract | ▴Top |
Sarcoidosis is a multisystem disorder characterized by granulomatous inflammation on histopathological evaluation. Diagnosis of sarcoidosis requires thorough elimination of malignancy and alternative causes of noncaseating granulomatous inflammation. Sarcoidosis and several subtypes of lymphoma have similar clinical presentations and can potentially have similar histopathological findings. Patients with a histopathology-confirmed diagnosis of sarcoidosis are at higher risk of developing malignancies. In this report, we present a case of a 64-year-old male diagnosed with sarcoidosis 2 years before presenting to the emergency department with a 4-month history of generalized weakness, cough, and very high fever. After a thorough workup involving cervical lymph node biopsy and bone marrow biopsy, he was diagnosed with peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS). Due to the patient’s current lymphoma diagnosis and features noted on pathology, a retrospective review of the prior biopsy specimen was performed, finding similar hematopathological features on both initial lymph node biopsy diagnosing sarcoidosis and current biopsies diagnosing lymphoma. Given these findings, our patient likely had early manifestation of PTCL misdiagnosed as sarcoidosis. In summary, lymphoma should be considered in all patients with suspected sarcoidosis, especially those who do not respond to treatment or who present with persistent hematological abnormalities.
Keywords: Peripheral T-cell lymphoma; Sarcoidosis; Sarcoidosis-lymphoma syndrome
| Introduction | ▴Top |
Sarcoidosis is a multisystem disorder characterized by granulomatous inflammation on histopathological evaluation of involved organs. The exact pathogenesis of sarcoidosis is an area of active scientific discovery, but there are studies examining the role of follicular regulatory T (Tfr) cell dysregulation [1]. Classically, sarcoidosis is known for pulmonary involvement, but among those with a disseminated clinical phenotype, there is a spectrum of disease manifestations from asymptomatic to a severe, progressive, and relapsing disease. Pulmonary involvement usually manifests as bilateral hilar adenopathy and reticular opacities leading to respiratory symptoms and fatigue as presenting symptoms [2]. Additional common presenting symptoms include cough, dyspnea, chest pain, fatigue, malaise, and weight loss. Patients over the age of 70 with sarcoidosis are more likely to present with systemic symptoms (fever, night sweats, and weight loss) [3]. According to the Clinical Practice Guideline by the American Thoracic Society (ATS) on the diagnosis of sarcoidosis, diagnostic criteria include: 1) “a compatible clinical presentation”, 2) noncaseating granulomatous inflammation on pathology, and 3) “exclusion of alternative causes of granulomatous disease” [4]. The differential diagnosis for granulomatous disease is broad and includes infectious causes (including bacterial, mycobacterial, and fungal etiologies) and noninfectious inflammatory conditions (including malignancy and rheumatologic conditions, among others). The ATS recommends against lymph node biopsies for routine diagnosis in asymptomatic patients; however, should the patient require treatment, they recommend biopsy via endobronchial ultrasound (EBUS)-guided lymph node biopsy [4]. Regardless of symptomatology, all patients with sarcoidosis should undergo annual complete blood count to screen for an evolving hematological malignancy [4]. Imaging, including EBUS for lymph node biopsy, chest radiography, and other modalities, such as fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG-PET/CT), has come to play a major role in monitoring therapeutic reaction to glucocorticoids and long-term prognosis [5].
There are numerous links between sarcoidosis and lymphoma. Granulomatous inflammation on histology can be a common feature in both diseases, with lymphomas rarely exhibiting this feature in published case reports [6-9]. It has been well established that patients with sarcoidosis are at higher risk of developing lymphoma (11.5 times the risk of the control population), as well as lung cancer (three times the risk) [10]. The association between sarcoidosis and lymphoma is known as sarcoidosis-lymphoma syndrome, with the development of sarcoidosis commonly preceding lymphoma [11-13]. In addition to lung cancer and lymphoma, patients with sarcoidosis are at an increased risk of developing other malignancies, including gastric, small intestine, hepatocellular, melanoma, non-melanoma skin cancer, additional non-Hodgkin lymphomas and leukemia [14]. The exact mechanism behind this association beyond underlying chronic inflammation leading to malignancy is still an active point of discovery. Here, we present the case of a patient previously diagnosed with sarcoidosis who was subsequently diagnosed by our team with peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS). In the workup of this new diagnosis, we aimed to review his prior diagnosis to determine if sarcoidosis was correct, finding features consistent with an underlying lymphoma matching our current diagnosis of PTCL, NOS. This case highlights the importance of keeping a broad differential and not anchoring on a diagnosis before excluding other possibilities.
| Case Report | ▴Top |
Investigations
A 64-year-old male with a past medical history significant for lung adenocarcinoma treated with radiation therapy (last treatment being 5 months prior to admission) currently in remission, coronavirus disease 2019 (COVID-19) infection (2 months prior to admission), pulmonary coccidioidomycosis (treated with 1 year of fluconazole therapy over 5 years ago), and sarcoidosis (currently treated with prednisone 10 mg PO daily) presented to the emergency department for a 4-month history of generalized weakness, cough, headache, and self-reported fever of 106 °F on the day of admission. Additionally, he reported having a sore throat twice in the last 2 months treated with amoxicillin and cefalexin that did not alleviate the symptoms.
He was initially diagnosed with sarcoidosis almost 2 years prior to this admission. His initial symptoms at that time were night sweats and noticeable inguinal lymphadenopathy with histopathological evaluation of the biopsied lymph node consistent with noncaseating granulomatous inflammation. A diagnosis of sarcoidosis was made at that time based on a negative workup for infectious causes at the time. His primary care physician was managing his sarcoidosis with prednisone. His was diagnosed with AJCC stage IA1 lung adenocarcinoma approximately 5 months prior to this admission after a right upper lobe lung mass was noted on chest imaging and EBUS-guided biopsy of regional lymph nodes was negative for malignancy or further spread. His lung adenocarcinoma responded to radiation therapy and remission was achieved. His most recent PET-CT showed new-onset FDG-avid lymphadenopathy. Of note, the patient’s social history was significant for occupational smoke exposure as a firefighter and significant smoking history of 3 - 4 cigars per day for 30 years.
On admission, his physical exam was remarkable for conjunctival pallor, dry mucous membranes, submandibular and inguinal lymphadenopathy, and hepatosplenomegaly. There were no focal neurological deficits. Initial laboratories showed pancytopenia with marked leukopenia/neutropenia (absolute neutrophil count of 670 cells/µL) and increased inflammatory markers with C-reactive protein elevated at 80.5 mg/L. He was admitted to the hospital for evaluation and management of pancytopenia with possible bone marrow failure of unknown etiology. He was started on empiric broad-spectrum antibiotics (vancomycin and piperacillin-tazobactam).
Diagnosis
An excisional right cervical lymph node biopsy and bone marrow biopsy were performed following resolution of fever (Fig. 1). Findings from both biopsies were consistent with a diagnosis of PTCL, NOS with presence of TRA/D gene rearrangement and negative staining for CD30. Due to the patient’s current lymphoma diagnosis and features noted on pathology, a retrospective review of his original inguinal lymph node biopsy diagnosing sarcoidosis was performed. Highlights of this investigation and comparison to current biopsy findings are discussed below in the “Discussion” section.
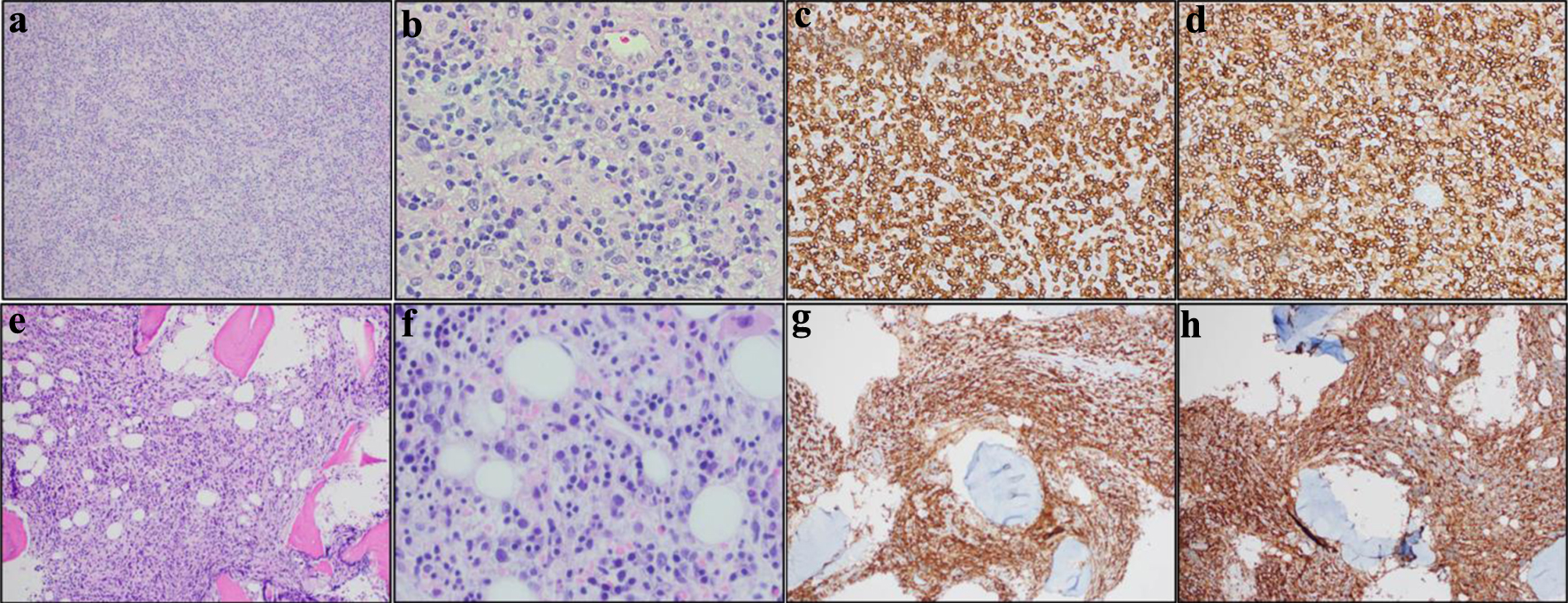 Click for large image | Figure 1. Cervical lymph node biopsy and bone marrow biopsy histology and immunohistochemistry confirming diagnosis of peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS). (a)-(d) are cervical lymph node biopsy and (e)-(h) are bone marrow biopsy. (a) H&E of diagnostic lymph node at × 100. Clusters of epithelioid histiocytes have now been infiltrated by neoplastic lymphoid cells. (b) H&E of diagnostic lymph node at × 400. The arrows point to examples of large neoplastic T cells. (c) CD3 immunostain at × 100. (d) CD4 immunostain at × 400. The neoplastic T cells are CD4-positive/CD8-negative. (e) H&E of bone marrow at × 100. (f) H&E of bone marrow at × 400. (g) CD3 immunostain at × 100. (h) CD4 immunostain at × 400. H&E: hematoxylin and eosin. |
Treatment, follow-up, and outcomes
Frontline lymphoma-directed therapy consisted of CHOEP (etoposide, cyclophosphamide, doxorubicin, vincristine and prednisone). Cycles consist of 3 weeks of etoposide (100 mg/m2 intravenously on days 1 - 3), cyclophosphamide (750 mg/m2 intravenously on day 1 after etoposide), doxorubicin (50 mg/m2 intravenously on day 1 after etoposide and cyclophosphamide), vincristine (2 mg intravenously on day 1 after etoposide, cyclophosphamide, and doxorubicin), and prednisone (100 mg orally on days 1 - 5) [15-17]. Partway through the first cycle of chemotherapy, our patient developed neutropenic fever, invasive Aspergillus sinusitis, and acute hypoxic respiratory failure requiring intubation. After a thorough goals of care discussion with the patient and his family post-extubation, he was discharged from the hospital to home hospice.
| Discussion | ▴Top |
Occasionally, lymphomas associated with granulomas have been misdiagnosed as sarcoidosis or other granulomatous diseases [9]. Sarcoidosis and lymphoma are both FDG-avid; thus, it is important to verify histology and have clinical acumen to avoid misdiagnosis before initiating therapy. Sarcoidosis and lymphoma may present at the same time in a patient which further complicates accurate diagnosis.
For our patient, it is likely that he had lymphoma at the time of initial sarcoidosis diagnosis. The patient’s excisional right cervical lymph node (Fig. 1a-d) showed replacement of nodal architecture by atypical lymphocytes with background histiocytes. These atypical lymphocytes expressed CD2 and CD5, expressed CD4 at a higher rate than CD8, expressed the TRA/D gene rearrangement, and lost expression of CD3 and CD7. The atypical lymphocyte karyotype showed tetraploidy, t(14,19), and del 6q. The patient’s bone marrow biopsy showed a similar abnormal T-cell infiltrate with similar immunophenotypic results (Fig. 1e-h). These findings were consistent with current diagnosis of PTCL, NOS, warranting retrospective review of his initial sarcoidosis diagnosis. Review of pathology slides from his initial inguinal lymph node biopsy 2 years ago showed an atypical T-cell infiltrate with scattered large T cells in a background of abundant epithelioid histiocytes (Fig. 2a-d). Abnormal mature CD4+ T cells were seen lacking surface CD3 and diminished CD7 on immunohistochemistry analysis (Fig. 2a-d). Molecular studies also showed similar clonal T-cell receptor gamma gene rearrangement. Given these similarities in the pathology, the initial lymph node biopsy could represent early manifestation of PTCL. Taken together, the lymphoepithelioid variant of PTCL, NOS should have been considered as a diagnosis at the time [18, 19] The patient’s rapid deterioration was likely multifactorial with a major contributor being the delay in diagnosis of lymphoma as well as the patient’s comorbidities including history of lung adenocarcinoma treated with radiation therapy. In learning from this case, lymphoma should be considered in all patients with suspected sarcoidosis, especially those who do not respond to treatment or who present with persistent hematological abnormalities [12].
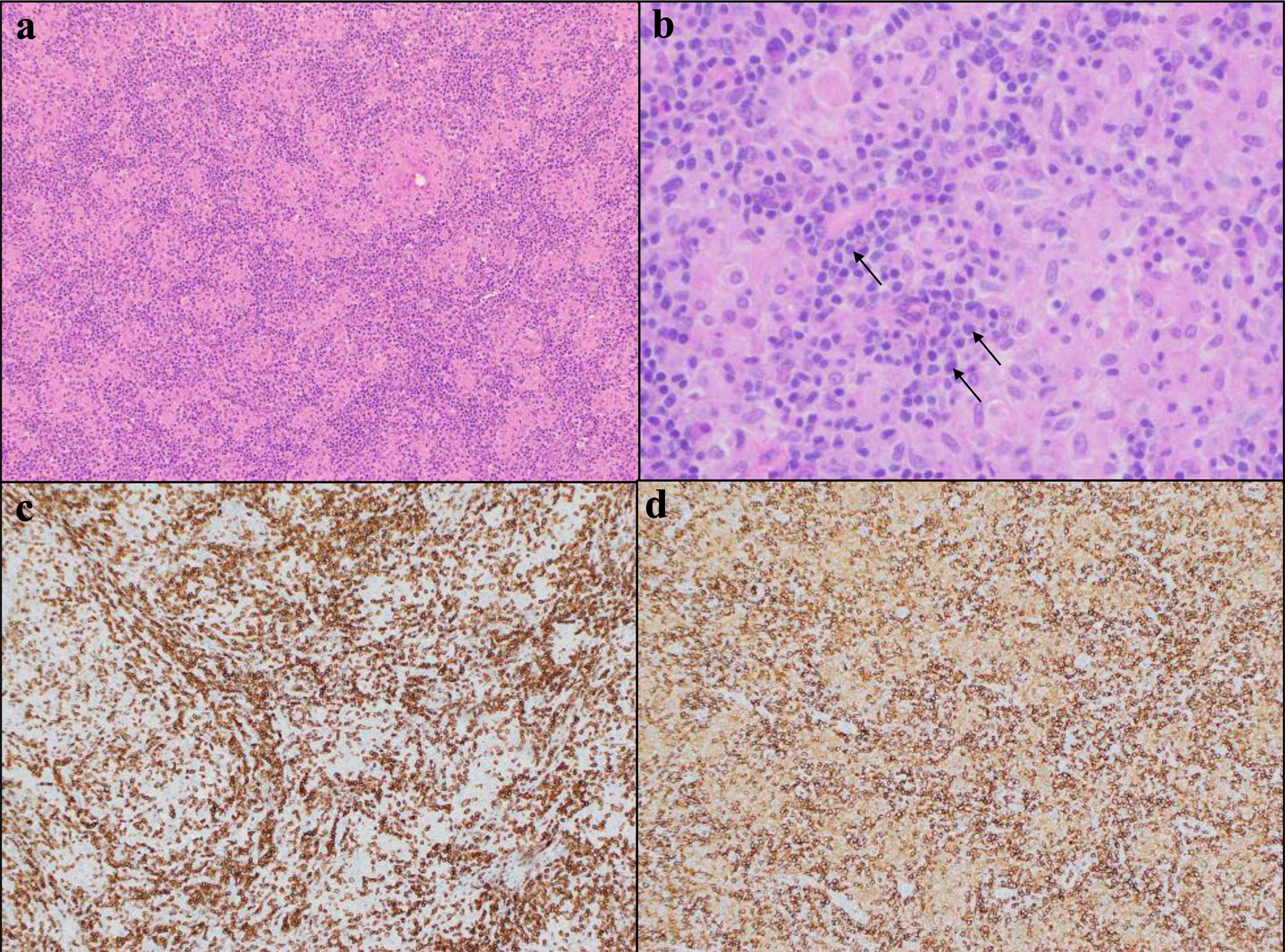 Click for large image | Figure 2. Outside lymph node biopsy from patient’s original diagnosis of sarcoidosis 2 years prior to admission. (a) H&E photograph of lymph node at × 100. (b) H&E of lymph node at × 400 with black arrows pointing to representative abnormal lymphocytes. (c) CD3 immunostain at × 100. (d) CD4 immunostain at × 400. H&E: hematoxylin and eosin. |
The patient’s lymphoma, classified according to the 2016 revised World Health Organization (WHO) classification of mature T- and natural killer (NK)-cell neoplasms, was PTCL, NOS with CD30- status. PTCL, NOS, encompasses a heterogenous group of mature T-cell lymphomas that do not meet criteria for other WHO-defined entities [20]. Based on genetic expression profiling analysis of PTCL, NOS, there are two distinct subgroups of mutations driving PTCL, NOS: mutations of transcriptional regulators GATA3 or TBX21 [20, 21]. Despite these two genetic subgroups, PTCL, NOS can have a number of other genetic driving factors, including expression of CD30, a member of the tumor necrosis factor (TNF) receptor superfamily that leads to downstream activation of nuclear factor-kappa B (NF-κB) [22]. CD30+ and CD30- PTCL, NOS have different gene expression and noticeable differences in immunohistochemistry [23, 24]. It has been shown that CD30- PTCL, NOS carry a worse prognosis and have worse clinical outcomes [25].
Learning points
In patients with clinical suspicion for sarcoidosis, it is imperative to rule out underlying malignancy. Given that the symptoms can overlap between the two, careful consideration and in-depth histopathological evaluation are warranted to correctly diagnose sarcoidosis or underlying leukemia/lymphoma. Additionally, given the ATS Clinical Practice Guidelines for the diagnosis of sarcoidosis, thorough exclusion of alternative causes of granulomatous disease is a diagnostic requirement [4]. In retrospect, our patient was unfortunately misdiagnosed and may have benefitted from earlier initiation of chemotherapy.
Acknowledgments
None to declare.
Financial Disclosure
All the above authors declare that they have received no financial considerations from any person or organization to support the preparation, analysis, results, or discussion of this article.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
SVM and JPH-D assisted the patient as medical students on the hematology/oncology inpatient service and co-wrote the manuscript. CW, AA, and AK are hematologist/oncologists who assisted the case as the primary inpatient medical team taking care of the patient. AH, DF, CYR and CS are hematopathologists extensively involved in the hematopathological investigation of this case, including review of outside pathology slides. All authors read and approved the final manuscript after thorough internal critical review for intellectual content. All authors agree to be accountable for all aspects of the work.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- d'Alessandro M, Bergantini L, Cameli P, Mezzasalma F, Refini RM, Pieroni M, Sestini P, et al. Adaptive immune system in pulmonary sarcoidosis-Comparison of peripheral and alveolar biomarkers. Clin Exp Immunol. 2021;205(3):406-416.
doi pubmed pmc - Wessendorf TE, Bonella F, Costabel U. Diagnosis of sarcoidosis. Clin Rev Allergy Immunol. 2015;49(1):54-62.
doi pubmed - Chevalet P, Clement R, Rodat O, Moreau A, Brisseau JM, Clarke JP. Sarcoidosis diagnosed in elderly subjects: retrospective study of 30 cases. Chest. 2004;126(5):1423-1430.
doi pubmed - Crouser ED, Maier LA, Wilson KC, Bonham CA, Morgenthau AS, Patterson KC, Abston E, et al. Diagnosis and detection of sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;201(8):e26-e51.
doi pubmed pmc - Chen H, Jin R, Wang Y, Li L, Li K, He Y. The Utility of (18)F-FDG PET/CT for Monitoring Response and Predicting Prognosis after Glucocorticoids Therapy for Sarcoidosis. Biomed Res Int. 2018;2018:1823710.
doi pubmed pmc - Du J, Zhang Y, Liu D, Zhu G, Zhang Q. Hodgkin's lymphoma with marked granulomatous reaction: a diagnostic pitfall. Int J Clin Exp Pathol. 2019;12(7):2772-2774.
pubmed pmc - Wu CY, Wang RC, Chen BJ, Chen WY, Jhuang JY, Chang MC, Wu YH, et al. Granuloma with an underlying lymphoma: a diagnostic challenge and a wider histologic spectrum including adult T-cell leukemia/lymphoma. Appl Immunohistochem Mol Morphol. 2020;28(4):316-324.
doi pubmed - Kunnumbrath A, Chandra H, Azad S, Balasubramanian P. Necrotising granulomas masking Hodgkin lymphoma: Report of a rare case. Hematol Transfus Cell Ther. 2023;45(Suppl 2):S157-S160.
doi pubmed pmc - Judson MA. Granulomatous sarcoidosis mimics. Front Med (Lausanne). 2021;8:680989.
doi pubmed pmc - Brincker H, Wilbek E. The incidence of malignant tumours in patients with respiratory sarcoidosis. Br J Cancer. 1974;29(3):247-251.
doi pubmed pmc - El Jammal T, Pavic M, Gerfaud-Valentin M, Jamilloux Y, Seve P. Sarcoidosis and cancer: a complex relationship. Front Med (Lausanne). 2020;7:594118.
doi pubmed pmc - Dal Lago L, Sarrand J, Woff E, Awada A, Vouche M, Pepersack T. Sarcoidosis versus lymphoma? Eur J Case Rep Intern Med. 2021;8(3):002250.
doi pubmed pmc - Matsuo T, Tanaka T, Omote R, Okada T, Notohara K, Okada K. Diffuse large B-cell lymphoma in the course of systemic sarcoidosis: A case report and review of 30 Japanese patients with sarcoidosis-lymphoma syndrome. J Clin Exp Hematop. 2022;62(4):226-237.
doi pubmed pmc - Askling J, Grunewald J, Eklund A, Hillerdal G, Ekbom A. Increased risk for cancer following sarcoidosis. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1668-1672.
doi pubmed - Pfreundschuh M, Trumper L, Kloess M, Schmits R, Feller AC, Rube C, Rudolph C, et al. Two-weekly or 3-weekly CHOP chemotherapy with or without etoposide for the treatment of elderly patients with aggressive lymphomas: results of the NHL-B2 trial of the DSHNHL. Blood. 2004;104(3):634-641.
doi pubmed - Pfreundschuh M, Trumper L, Kloess M, Schmits R, Feller AC, Rudolph C, Reiser M, et al. Two-weekly or 3-weekly CHOP chemotherapy with or without etoposide for the treatment of young patients with good-prognosis (normal LDH) aggressive lymphomas: results of the NHL-B1 trial of the DSHNHL. Blood. 2004;104(3):626-633.
doi pubmed - Trumper L, Zwick C, Ziepert M, Hohloch K, Schmits R, Mohren M, Liersch R, et al. Dose-escalated CHOEP for the treatment of young patients with aggressive non-Hodgkin's lymphoma: I. A randomized dose escalation and feasibility study with bi- and tri-weekly regimens. Ann Oncol. 2008;19(3):538-544.
doi pubmed - Etebari M, Navari M, Agostinelli C, Visani A, Peron C, Iqbal J, Inghirami G, et al. Transcriptional analysis of lennert lymphoma reveals a unique profile and identifies novel therapeutic targets. Front Genet. 2019;10:780.
doi pubmed pmc - Cho U, Park G, Kim JA, Im S. Lymphoepithelioid variant of peripheral T cell lymphoma (Lennert lymphoma): Cytologic and histologic features. Diagn Cytopathol. 2021;49(2):322-324.
doi pubmed - Hathuc V, Kreisel F. Genetic landscape of peripheral T-cell lymphoma. Life (Basel). 2022;12(3):410.
doi pubmed pmc - Iqbal J, Wright G, Wang C, Rosenwald A, Gascoyne RD, Weisenburger DD, Greiner TC, et al. Gene expression signatures delineate biological and prognostic subgroups in peripheral T-cell lymphoma. Blood. 2014;123(19):2915-2923.
doi pubmed pmc - van der Weyden CA, Pileri SA, Feldman AL, Whisstock J, Prince HM. Understanding CD30 biology and therapeutic targeting: a historical perspective providing insight into future directions. Blood Cancer J. 2017;7(9):e603.
doi pubmed pmc - Bisig B, de Reynies A, Bonnet C, Sujobert P, Rickman DS, Marafioti T, Delsol G, et al. CD30-positive peripheral T-cell lymphomas share molecular and phenotypic features. Haematologica. 2013;98(8):1250-1258.
doi pubmed pmc - Sabattini E, Pizzi M, Tabanelli V, Baldin P, Sacchetti CS, Agostinelli C, Zinzani PL, et al. CD30 expression in peripheral T-cell lymphomas. Haematologica. 2013;98(8):e81-82.
doi pubmed pmc - Broccoli A, Zinzani PL. Peripheral T-cell lymphoma, not otherwise specified. Blood. 2017;129(9):1103-1112.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


